The gallbladder is a small, pear-shaped organ tucked beneath the liver that stores and releases bile to aid in digestion, particularly of fats. While it plays a role in digestive function, it’s not essential for survival. In fact, millions of people live healthy lives without one. However, when the gallbladder becomes diseased or dysfunctional, removal—known as cholecystectomy—may be the best medical solution. Understanding why this procedure is performed, what symptoms signal trouble, and when intervention is necessary can help patients make informed decisions about their health.
Common Reasons for Gallbladder Removal
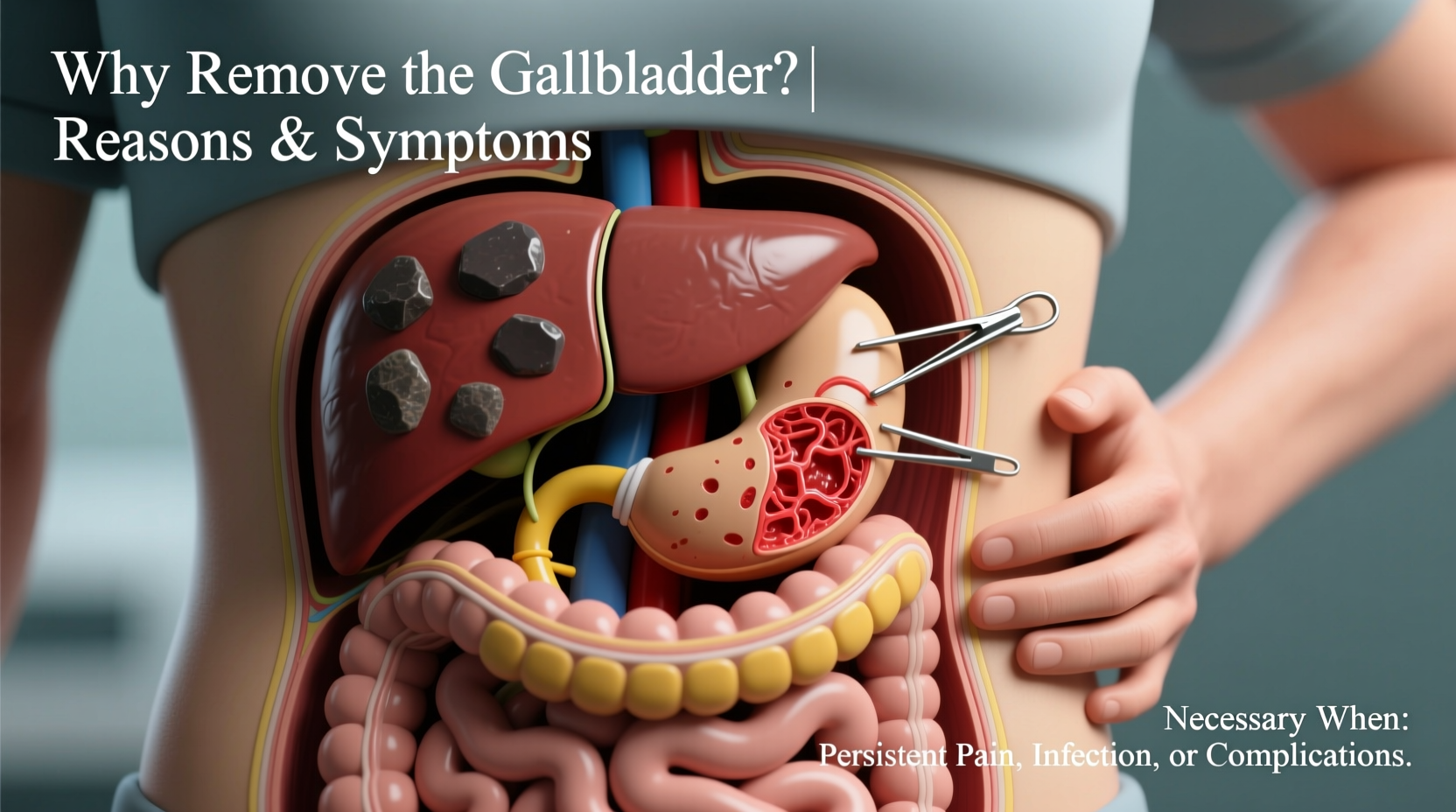
Gallbladder removal is typically recommended when the organ causes recurring pain, inflammation, or complications due to underlying conditions. The most frequent reasons include:
- Gallstones (Cholelithiasis): Hardened deposits of digestive fluid that form in the gallbladder. They can block bile ducts, leading to severe pain and infection.
- Cholecystitis: Inflammation of the gallbladder, often caused by gallstones blocking the cystic duct. Acute cases require prompt treatment; chronic inflammation may lead to long-term damage.
- Biliary Colic: Intermittent pain caused by temporary blockage of bile flow, usually from a gallstone passing through the duct system.
- Pancreatitis: In some cases, gallstones migrate to the common bile duct and trigger inflammation of the pancreas, a serious condition requiring gallbladder removal to prevent recurrence.
- Gallbladder Polyps or Tumors: Growths larger than 1 cm carry an increased risk of cancer and often warrant surgical removal even if asymptomatic.
- Acalculous Gallbladder Disease: A condition where the gallbladder doesn’t empty properly despite no stones being present, causing chronic pain.
Symptoms That Signal Gallbladder Problems
Early recognition of symptoms can prevent complications such as infection or organ rupture. Common signs that something is wrong with the gallbladder include:
- Sharp pain in the upper right abdomen, often radiating to the back or shoulder blade
- Nausea and vomiting, particularly after meals
- Bloating, gas, and indigestion
- Fever or chills (indicative of infection)
- Jaundice (yellowing of skin or eyes), which suggests bile duct obstruction
- Clay-colored stools and dark urine—signs of impaired bile flow
Symptoms frequently occur after consuming greasy or heavy foods, as these stimulate the gallbladder to release bile. Over time, repeated episodes can progress from mild discomfort to acute emergencies.
“Patients often mistake gallbladder pain for heartburn or indigestion. But persistent post-meal pain on the right side should never be ignored.” — Dr. Lena Torres, Gastroenterologist
When Is Surgery Necessary?
Not everyone with gallstones requires surgery. Many remain asymptomatic and are diagnosed incidentally during imaging for other conditions. However, once symptoms develop, the likelihood of future complications increases significantly. Surgery becomes necessary under the following circumstances:
- Recurrent Biliary Pain: Two or more episodes of significant pain linked to gallstones.
- Acute Cholecystitis: Confirmed via ultrasound or HIDA scan, usually requiring hospitalization and prompt removal within 72 hours.
- Common Bile Duct Obstruction: When stones migrate and block bile flow, leading to jaundice or pancreatitis.
- Gallbladder Dysfunction: A HIDA scan showing ejection fraction below 35–40% indicates poor function and justifies removal.
- Risk of Cancer: Presence of large polyps (>1 cm), porcelain gallbladder (calcified walls), or family history of biliary cancers.
Laparoscopic cholecystectomy—the minimally invasive approach—is the gold standard, offering quicker recovery and fewer complications compared to open surgery.
Step-by-Step: What to Expect Before and After Surgery
Understanding the surgical journey helps reduce anxiety and ensures better preparation and recovery.
Pre-Operative Phase
- Medical evaluation including blood work, imaging (ultrasound, CT, or MRI), and possibly a HIDA scan.
- Fasting for at least 8 hours before surgery.
- Review of medications—blood thinners may need to be paused.
During Surgery
- Anesthesia is administered (general).
- Four small incisions are made; a laparoscope and surgical tools are inserted.
- The gallbladder is detached and removed through one of the ports.
- Duration: Typically 60–90 minutes.
Post-Operative Recovery
- Most patients go home the same day.
- Mild pain at incision sites and shoulder tip pain (from gas used during surgery) are common but resolve within days.
- Resume light activities within a few days; avoid heavy lifting for 2–4 weeks.
- Dietary adjustments: Start with low-fat foods and gradually reintroduce fats as tolerated.
Do’s and Don’ts After Gallbladder Removal
| Do’s | Don’ts |
|---|---|
| Eat small, frequent meals rich in fiber | Consume large, fatty meals immediately after surgery |
| Stay hydrated and increase water intake | Ignore persistent diarrhea or severe abdominal pain |
| Gradually test tolerance to healthy fats like avocado or olive oil | Resume intense physical activity too soon |
| Follow up with your surgeon in 1–2 weeks | Stop prescribed medications without consulting your doctor |
Real-Life Example: Recognizing the Warning Signs
Sarah, a 45-year-old teacher, began experiencing sharp pains in her upper abdomen after dinner, often waking her at night. She initially attributed it to spicy food or stress. Over several months, the episodes became more frequent and were accompanied by nausea and bloating. After one particularly severe attack lasting over six hours, she visited the emergency room. An ultrasound revealed multiple gallstones and thickening of the gallbladder wall—signs of chronic cholecystitis. Her doctor recommended surgery. Within a week of laparoscopic removal, Sarah reported immediate relief. Six weeks later, she had resumed normal activities and adjusted her diet to include moderate fats without discomfort.
Sarah’s case illustrates how seemingly minor digestive complaints can escalate into a clear medical need for intervention.
Frequently Asked Questions
Can you live a normal life without a gallbladder?
Yes. The liver continues to produce bile, which flows directly into the small intestine. Most people adapt well, though some may experience temporary changes in digestion, such as looser stools after fatty meals. These usually improve over time.
Will I have to follow a strict diet forever after surgery?
No. While a low-fat diet is recommended initially, many patients can eventually return to a balanced diet. Long-term restrictions are rarely necessary unless individual intolerance persists.
What are the risks of not removing a diseased gallbladder?
Leaving a symptomatic gallbladder untreated increases the risk of complications such as gangrene, perforation, sepsis, recurrent pancreatitis, or obstructive jaundice—all of which can be life-threatening.
Conclusion: Taking Charge of Your Digestive Health
Deciding to remove the gallbladder is not taken lightly, but when symptoms persist or complications arise, surgery offers a definitive solution. From gallstones to chronic inflammation, timely intervention prevents serious health risks and restores quality of life. Pay attention to your body’s signals, seek medical evaluation for persistent abdominal pain, and work with your healthcare provider to determine the best course of action.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?