Corticosteroids like prednisone are powerful anti-inflammatory medications used to treat a wide range of conditions—from asthma and autoimmune diseases to severe allergies and certain cancers. While effective, these drugs suppress the body’s natural hormone production. When taken for more than a few weeks, abruptly stopping them can lead to life-threatening complications. That’s why healthcare providers use a tapering strategy: gradually reducing the dose over time. Understanding this process is essential for patient safety and recovery.
The Role of Cortisol in the Body
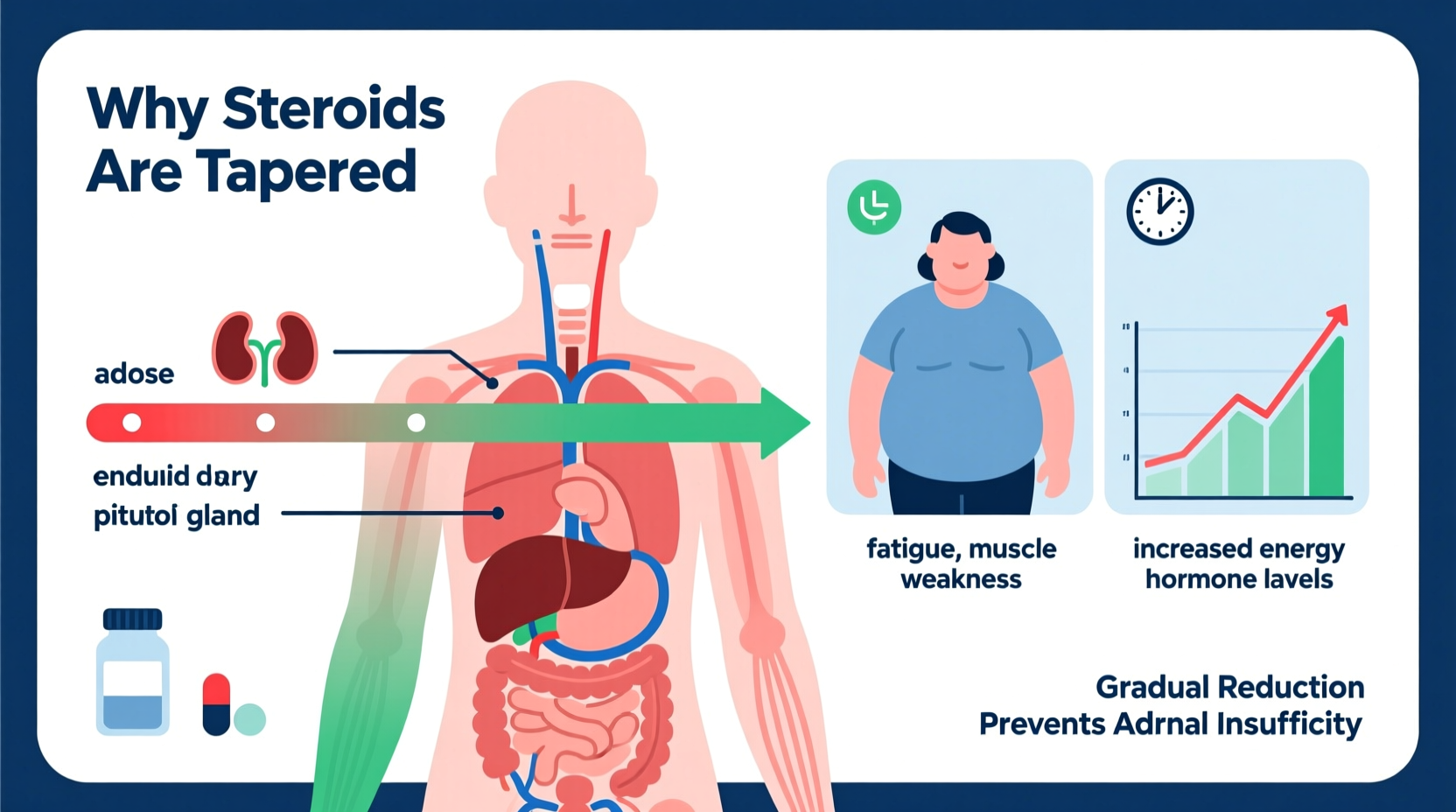
The human body produces cortisol—a steroid hormone—through the adrenal glands. This hormone helps regulate metabolism, immune response, blood pressure, and stress adaptation. The hypothalamus and pituitary gland in the brain control cortisol release through a feedback loop known as the HPA axis (hypothalamic-pituitary-adrenal axis).
When a person takes external corticosteroids for an extended period, the brain senses high steroid levels and signals the adrenal glands to stop producing cortisol. Over time, the adrenal glands “go to sleep,” becoming inactive due to lack of stimulation. If the medication is stopped suddenly, the body has no internal cortisol and no external supply—leading to acute adrenal insufficiency.
“Stopping steroids cold turkey after prolonged use is one of the most dangerous mistakes a patient can make. The adrenals need time to wake back up.” — Dr. Lena Patel, Endocrinologist at Boston Medical Center
Why Tapering Is Necessary
Tapering allows the HPA axis to recover gradually. By slowly decreasing the steroid dose, the brain begins to detect lower hormone levels and resumes signaling the adrenal glands to produce cortisol naturally. This reactivation process can take days to months, depending on treatment duration and dosage.
Without tapering, patients risk developing adrenal crisis—a medical emergency characterized by severe fatigue, low blood pressure, vomiting, confusion, and even shock. In rare cases, it can be fatal.
Factors That Influence Tapering Duration
No single tapering schedule fits all patients. Several factors determine how quickly or slowly steroids should be reduced:
- Duration of therapy: Patients on steroids for over 3 weeks typically require tapering; those on longer regimens may need several months.
- Dosage: Higher doses suppress adrenal function more severely, requiring slower tapers.
- Underlying condition: Diseases like lupus or vasculitis may flare if steroids are reduced too quickly.
- Individual response: Some people regain adrenal function faster than others.
- Route of administration: Oral and intravenous steroids have systemic effects and usually require tapering; topical or inhaled forms often do not.
A Real-World Example: Managing Prednisone After Severe Asthma Exacerbation
Sarah, a 45-year-old teacher, was hospitalized with a severe asthma attack. She received intravenous methylprednisolone for five days, followed by a 6-week course of oral prednisone starting at 40 mg daily. Her pulmonologist prescribed a taper: reducing by 5 mg every week until reaching 20 mg, then slowing to 2.5 mg reductions every 1–2 weeks.
At week 8, Sarah felt well and stopped her medication early, assuming she no longer needed it. Within three days, she developed dizziness, nausea, joint pain, and profound weakness. She returned to her doctor, who diagnosed adrenal insufficiency. Restarting prednisone and resuming the taper corrected her symptoms. This case highlights how even well-intentioned patients can face serious consequences when skipping the taper.
Step-by-Step Guide to Steroid Tapering
Tapering must be personalized, but follows general principles. Below is a typical framework for oral prednisone after long-term use (e.g., >20 mg/day for >4 weeks):
- Assessment: Confirm the need for tapering based on treatment length, dose, and disease stability.
- Baseline plan: Develop a schedule with the prescribing physician—weekly reductions initially, then slower as lower doses are reached.
- Monitor symptoms: Track energy levels, blood pressure, joint pain, and signs of relapse or adrenal insufficiency.
- Adjust as needed: If symptoms worsen (e.g., inflammation returns), pause or slow the taper.
- Final phase: Below 10 mg/day, reductions may occur every 1–2 weeks. Doses under 5 mg/day may be maintained for weeks before discontinuation.
- Follow-up: Some patients benefit from cortisol level testing post-taper to confirm adrenal recovery.
Common Tapering Schedules Compared
| Starting Dose | Taper Duration | Reduction Pattern | Best For |
|---|---|---|---|
| 60 mg/day | 8–12 weeks | Reduce by 10 mg/week to 20 mg, then 5 mg every 1–2 weeks | Autoimmune flares (e.g., rheumatoid arthritis) |
| 40 mg/day | 6–10 weeks | 5 mg weekly reductions until 20 mg, then 2.5 mg every 1–2 weeks | Moderate asthma or allergic reactions |
| 20 mg/day | 4–6 weeks | 2.5–5 mg reductions every 1–2 weeks | Shorter courses with partial suppression |
| 10 mg/day | 2–4 weeks | 1–2.5 mg reductions weekly | Final phase of any long-term regimen |
Potential Complications of Improper Tapering
Rushing or skipping the taper exposes patients to two major risks:
- Adrenal Insufficiency: Symptoms include fatigue, nausea, low blood pressure, salt craving, and hypoglycemia. In severe cases, adrenal crisis requires emergency hydrocortisone injection.
- Disease Relapse: Conditions like Crohn’s disease, multiple sclerosis, or polymyalgia rheumatica can rebound aggressively if steroids are withdrawn too fast.
Conversely, tapering too slowly can expose patients to prolonged steroid side effects: weight gain, osteoporosis, elevated blood sugar, cataracts, and mood disturbances.
Do’s and Don’ts During Steroid Tapering
| Do’s | Don’ts |
|---|---|
| Follow your doctor’s tapering schedule precisely | Stop taking steroids abruptly |
| Carry a steroid alert card or wear medical ID | Double-dose if you miss a pill |
| Report new or worsening symptoms immediately | Self-adjust the taper without medical advice |
| Stay consistent with meals and sleep | Ignore signs of infection or stress |
Frequently Asked Questions
Can I skip the taper if I feel fine?
No. Feeling well does not mean your adrenal glands have recovered. Even asymptomatic patients can develop adrenal crisis after abrupt discontinuation. Always complete the prescribed taper.
How do I know if my adrenals have recovered?
Most people regain normal function within weeks to months. A morning cortisol blood test or ACTH stimulation test can assess adrenal responsiveness if symptoms persist post-taper.
What should I do during illness or stress while tapering?
During infections, surgery, or major stress, your body needs more cortisol. Your doctor may advise temporarily increasing your steroid dose—a process called “stress dosing.” Always have a sick-day plan in place.
Conclusion: Safety First in Steroid Management
Understanding why steroids are tapered is crucial for anyone prescribed long-term corticosteroid therapy. The taper isn’t just a formality—it’s a physiological necessity that protects your endocrine system and overall health. By respecting the process, monitoring symptoms, and maintaining open communication with your healthcare provider, you can safely discontinue steroids and regain hormonal balance.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?