For centuries, the microscope has been a cornerstone of microbiology, offering humanity its first glimpse into the invisible world of microorganisms. While visual inspection through microscopy remains a valuable tool, relying solely on visualization to identify bacteria is fundamentally flawed. Despite advances in imaging technology, morphology—how bacteria look under the lens—provides only superficial clues. True bacterial identification demands more than sight; it requires biochemical, genetic, and physiological analysis. Understanding why visualization falls short is critical for researchers, clinicians, and public health professionals who depend on accurate microbial identification.
The Limits of Morphological Identification
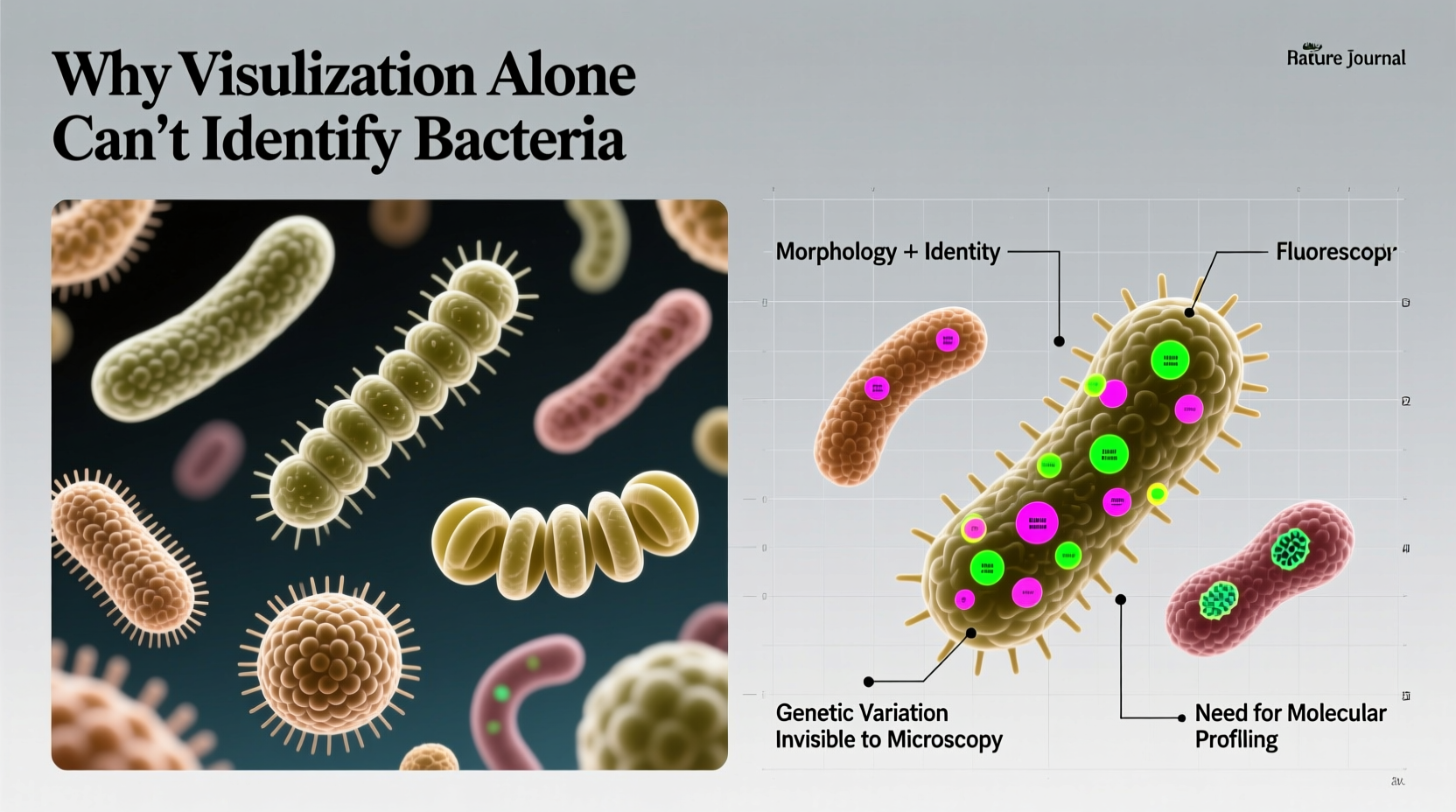
Under a light microscope, bacteria are typically categorized by shape: cocci (spherical), bacilli (rod-shaped), or spirilla (spiral). Arrangement—such as chains, clusters, or pairs—also offers basic classification. However, these traits are not unique to specific species. For example, Staphylococcus aureus and Staphylococcus epidermidis appear nearly identical under the microscope—both are gram-positive cocci in clusters. Yet one causes life-threatening infections, while the other is a common skin commensal.
Morphology does not reveal metabolic activity, virulence factors, antibiotic resistance, or genetic lineage. Two bacteria that look identical may belong to entirely different genera with vastly different clinical implications. This superficial level of analysis is insufficient for diagnosis, treatment planning, or epidemiological tracking.
Structural Similarities Across Diverse Species
Many bacterial species share similar cellular structures, especially within the same phylum. The Gram stain, a foundational technique in microbiology, classifies bacteria based on cell wall composition. But even this method has significant limitations. Gram-positive organisms like Bacillus and Listeria both appear as rod-shaped cells, yet their pathogenicity, environmental resilience, and treatment protocols differ drastically.
Moreover, some bacteria exhibit variable staining patterns. Haemophilus influenzae, for instance, may appear Gram-negative but is notoriously difficult to visualize without special staining due to its small size and tendency to form pleomorphic shapes. In chronic infections, bacteria like Pseudomonas aeruginosa can adopt filamentous forms under stress, misleading observers about their true identity.
“Morphology is a starting point, not an endpoint. Assuming identity from shape is like diagnosing a disease by silhouette.” — Dr. Lena Torres, Clinical Microbiologist, Johns Hopkins Hospital
Hidden Diversity: The Role of Biochemical and Genetic Profiling
To accurately identify bacteria, scientists must move beyond what the eye can see. Biochemical tests assess metabolic capabilities—such as whether a bacterium ferments lactose, produces catalase, or reduces nitrates. These functional traits help differentiate species that look alike. For example, Escherichia coli and Klebsiella pneumoniae are both Gram-negative rods, but only E. coli typically produces indole from tryptophan.
In modern labs, matrix-assisted laser desorption/ionization time-of-flight (MALDI-TOF) mass spectrometry analyzes protein profiles to identify bacteria rapidly and accurately. More advanced still is 16S rRNA gene sequencing, which compares genetic markers across species. This method can distinguish between organisms with identical morphology but divergent evolutionary histories.
| Bacterial Pair | Visual Similarity | Key Differentiating Factor | Identification Method Needed |
|---|---|---|---|
| Streptococcus pyogenes vs Streptococcus agalactiae | Both are Gram-positive cocci in chains | Hemolysis pattern & antigen type | Agglutination test / PCR |
| Salmonella spp. vs Shigella spp. | Gram-negative rods, indistinguishable visually | Lactose fermentation & motility | TSI agar / Motility test |
| Mycobacterium tuberculosis vs Mycobacterium avium | Both acid-fast bacilli | Growth rate & host preference | Culture + DNA probes |
Case Study: Misdiagnosis Due to Reliance on Visualization
In 2019, a rural clinic in India reported an outbreak of suspected cholera after identifying curved, motile Gram-negative rods in stool samples. Based on morphology and endemic history, clinicians initiated mass treatment with oral rehydration and doxycycline. However, laboratory confirmation at a regional center revealed the organism was actually Aeromonas hydrophila, not Vibrio cholerae. Though both appear similar under the microscope, Aeromonas exhibits intrinsic resistance to certain antibiotics and often causes extraintestinal infections.
The misidentification delayed targeted therapy for severe cases and led to unnecessary antibiotic use, increasing local resistance pressure. This case underscores how visual assumptions—even when supported by staining—can lead to flawed public health responses.
Step-by-Step: From Sample to Accurate Identification
Proper bacterial identification follows a structured workflow that transcends visualization. Here’s how it should be done:
- Sample Collection: Obtain specimen using sterile technique to prevent contamination.
- Direct Smear and Staining: Perform Gram or acid-fast stain for preliminary assessment.
- Culturing: Inoculate on selective and differential media (e.g., MacConkey agar) to isolate colonies.
- Colony Morphology Review: Note color, texture, hemolysis—but do not assume identity.
- Biochemical Testing: Run catalase, oxidase, API strips, or automated systems like VITEK.
- Molecular Confirmation: Use PCR, 16S sequencing, or MALDI-TOF for definitive ID.
- Antibiogram: Test susceptibility to guide treatment.
This sequence ensures that visual data informs—but does not dictate—the final conclusion.
Frequently Asked Questions
Can electron microscopy solve the problem of bacterial misidentification?
No. While electron microscopy provides ultra-high resolution images of surface structures and internal organelles, it still only reveals morphology. It cannot determine genetic makeup, metabolic function, or antibiotic resistance. Additionally, it's expensive, time-consuming, and impractical for routine diagnostics.
Are there any bacteria that can be reliably identified by sight alone?
Rarely. Even well-known forms like Neisseria gonorrhoeae (Gram-negative diplococci inside white blood cells) require culture or nucleic acid amplification tests (NAATs) for confirmation. Visual clues can raise suspicion, but never replace definitive testing.
Why not just use DNA testing for everything instead of looking at samples?
DNA-based methods are powerful but not always accessible in resource-limited settings. Microscopy provides rapid, low-cost preliminary data. The key is integrating visualization as part of a broader diagnostic strategy—not treating it as conclusive evidence.
Essential Checklist for Reliable Bacterial Identification
- ✅ Perform initial Gram stain for orientation
- ✅ Culture on appropriate media to isolate pure colonies
- ✅ Conduct biochemical tests relevant to suspected organisms
- ✅ Use automated or molecular systems for precise species-level ID
- ✅ Confirm antibiotic resistance patterns with susceptibility testing
- ✅ Cross-reference results with patient clinical presentation
Conclusion: Seeing Isn’t Believing in Microbiology
Visualization is indispensable in microbiology—it guides sample processing, helps assess specimen quality, and offers rapid preliminary insights. But equating appearance with identity is a dangerous oversimplification. Bacteria defy easy categorization by sight alone. Their diversity lies not in shape, but in function, genetics, and behavior. Accurate identification protects patients, informs public health, and combats antimicrobial resistance.
Whether you're a student, clinician, or researcher, remember: the microscope opens the door, but only comprehensive analysis can reveal the truth behind the slide.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?