N95 respirators are among the most effective personal protective equipment (PPE) for filtering airborne particles, including viruses like SARS-CoV-2. Originally designed for single use in industrial and medical settings, widespread demand during public health emergencies has led many individuals and institutions to consider reusing these masks. But is it safe? And if so, how many times can an N95 be reused before it stops offering reliable protection?
The answer isn't a simple yes or no. It depends on proper handling, storage, contamination risk, and environmental conditions. This article explores the science behind N95 filtration, real-world reuse practices, expert recommendations, and practical steps to extend mask life without compromising safety.
How N95 Masks Work: The Science Behind Filtration
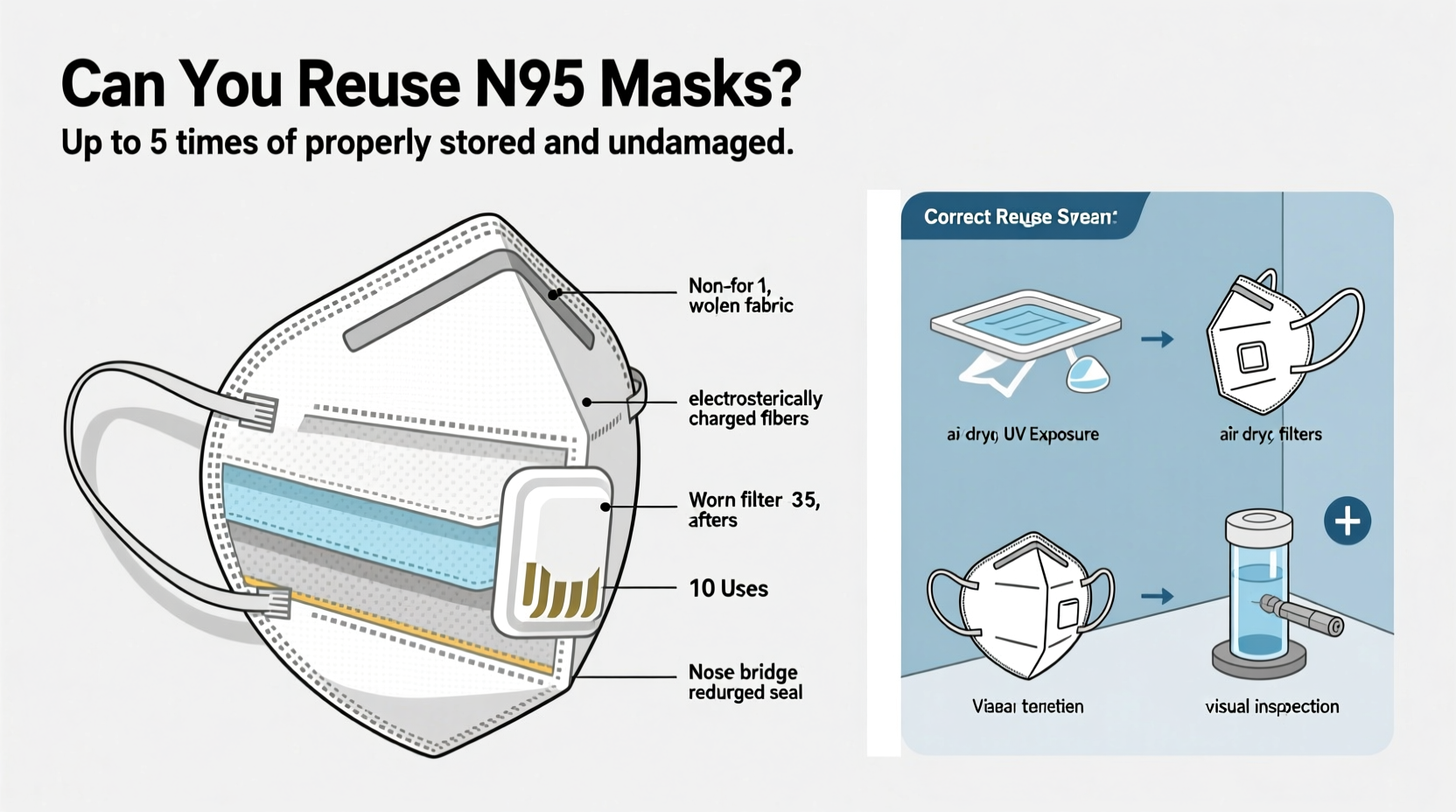
N95 respirators filter at least 95% of airborne particles that are 0.3 microns in size—the most penetrating particle size (MPPS). They achieve this through a combination of mechanical and electrostatic mechanisms:
- Mechanical filtration: Fibers in the mask physically block larger particles via interception and impaction.
- Electrostatic attraction: The polypropylene material carries a static charge that attracts smaller particles, enhancing capture efficiency.
This dual mechanism allows N95s to trap not only dust and aerosols but also pathogens such as viruses and bacteria. However, repeated use, moisture exposure, and improper handling can degrade both the physical structure and electrostatic properties of the filter layer.
“N95s rely on both fit and filtration integrity. Any compromise in either reduces protection significantly.” — Dr. Lisa Delano, Industrial Hygienist at NIOSH
Can You Reuse an N95 Mask Safely?
Under specific conditions, limited reuse of N95 masks is acceptable—even recommended by health authorities during shortages. The U.S. Centers for Disease Control and Prevention (CDC) and the National Institute for Occupational Safety and Health (NIOSH) have issued guidance allowing healthcare workers to reuse certain models under crisis capacity strategies.
However, \"reuse\" does not mean continuous wear over multiple days. Instead, it refers to using the same respirator for multiple encounters with patients or contaminated environments, provided it remains intact, functional, and uncontaminated between uses.
Key factors determining safe reuse include:
- Physical condition: No visible damage, deformation, or soiling.
- Filtration performance: Electrostatic charge retention and structural integrity.
- Fit seal: Must still form a tight seal around the nose and mouth.
- Contamination level: Not exposed to bodily fluids, high-risk aerosols, or infectious environments.
In non-healthcare settings—such as commuting, shopping, or home care—individuals may safely reuse their N95s if precautions are followed. The primary goal is to prevent self-contamination and maintain performance.
Recommended Number of Reuses Before Replacement
There is no universal number of safe reuses because it depends on usage context, storage, and model design. However, research and official guidelines suggest practical limits:
| Usage Context | Recommended Max Reuses | Conditions |
|---|---|---|
| Healthcare (controlled) | 5–10 cycles | Rotated with other masks; stored properly; inspected each time |
| Community Use (low risk) | 5 uses | No soiling, good storage, minimal touching |
| High-Risk Exposure | Single use only | Contact with infected persons or contaminated surfaces |
| Damaged or Wet Mask | Immediately discard | After any visible degradation or moisture exposure |
A study published in *The Journal of Hospital Infection* (2020) tested five common N95 models after repeated donning and doffing. Results showed that filtration efficiency remained above 95% for up to five uses when masks were handled carefully and stored in breathable paper bags between wears. Beyond seven uses, some models showed reduced fit due to strap elasticity loss.
Therefore, a conservative guideline is to limit reuse to **no more than five times** in low-exposure settings, assuming no damage, soiling, or moisture accumulation occurs.
Step-by-Step Guide to Safe N95 Reuse
If you plan to reuse your N95 mask, follow this evidence-based protocol to maximize safety and longevity:
- Wash hands thoroughly before handling the mask.
- Inspect the respirator for tears, stretched straps, or dirt. Discard if compromised.
- Put on the mask correctly: Pinch the nose bridge, ensure full coverage from nose to chin.
- Perform a user seal check every time by covering the mask and inhaling/exhaling sharply.
- After use, remove by the ear loops or head straps without touching the front.
- Store in a clean, dry place: Place in a breathable paper bag labeled with date and time of last use.
- Allow at least 48 hours between uses to let potential pathogens degrade naturally.
- Replace after 5 uses or sooner if fit feels loose, breathing becomes difficult, or visible wear appears.
What Damages N95 Performance?
Several factors accelerate the decline in N95 effectiveness:
- Moisture: Breathing, sweat, or humidity neutralizes the electrostatic charge in the filter media.
- Oils: Skin oils, makeup, or facial hair interfere with the face seal and degrade foam components.
- Physical deformation: Folding, crushing, or improper storage alters shape and fit.
- UV light and heat: Prolonged sun exposure breaks down polymers in the mask layers.
- Cleaning attempts: Washing with soap, alcohol, or bleach destroys the electrostatic layer and fibers.
Because the electrostatic charge cannot be restored once lost, cleaning methods that involve liquids generally render the mask ineffective—even if it looks intact.
Mini Case Study: Nurse Reusing N95s During a Pandemic Surge
During the winter surge of 2022, Maria, an ICU nurse in Chicago, faced persistent N95 shortages. Her hospital implemented a rotation system: staff were issued three certified N95s (3M 1860), which they reused over a two-week period following CDC guidelines.
Maria stored her masks in individual paper bags labeled Day 1, Day 2, and Day 3. After each shift, she hung the used mask in a designated clean area away from patient zones. She performed visual checks and seal tests daily. By rotating masks and allowing 72 hours between uses, she extended each respirator’s life to eight shifts without noticeable fit issues.
When one mask developed a small tear near the strap anchor, she immediately retired it. Her approach balanced safety, compliance, and resource conservation—demonstrating that structured reuse can work under pressure.
Do’s and Don’ts of N95 Reuse
| Do’s | Don’ts |
|---|---|
| Inspect mask before each use | Wash or disinfect with liquids |
| Store in a breathable container | Fold or crush the mask |
| Rotate multiple masks | Share your mask with others |
| Discard after 5 uses or damage | Use if visibly soiled or wet |
| Wash hands before and after handling | Touch the filter surface |
Expert Insight: What Health Organizations Say
The CDC acknowledges that during supply shortages, extended use and limited reuse of N95s are acceptable strategies. Their guidance emphasizes:
“Extended use is preferred over reuse when feasible, as it minimizes contact with potentially contaminated surfaces.” — CDC Interim Guidance, 2023
NIOSH adds that while most N95s are labeled for single use, “limited reuse” is permissible under controlled conditions. They stress that users must inspect for damage, maintain hygiene, and avoid decontamination methods that compromise filter integrity.
The World Health Organization (WHO) advises against reuse in high-transmission areas unless no alternatives exist. When reuse is necessary, WHO recommends strict adherence to storage, inspection, and replacement protocols.
FAQ: Common Questions About N95 Reuse
Can I clean my N95 mask with alcohol or soap?
No. Liquid-based cleaning agents—including hand sanitizer, soap, and bleach—damage the electrostatic charge and structural fibers of the mask. Once washed, the filtration efficiency drops below 95%, rendering it no longer an N95. Dry methods like UV irradiation or heat treatment exist but require specialized equipment and are not recommended for general consumers.
How do I know when to throw out my N95?
Discard your mask if: it no longer forms a tight seal; breathing feels harder; there’s visible dirt, tears, or odor; or it has been worn more than five times. Also discard immediately after close contact with someone who is sick or in a heavily polluted environment.
Is it safe to reuse an N95 at home?
Yes, in low-risk situations—like occasional travel or grocery shopping—reusing an N95 up to five times is generally safe if stored properly and not contaminated. Avoid reuse if you’re immunocompromised or caring for someone ill.
Conclusion: Balancing Safety and Practicality
Reusing N95 masks can be done safely, but only with discipline and awareness. While designed for single use, real-world constraints make limited reuse a viable option when managed correctly. Key practices—rotating multiple masks, storing them in breathable containers, avoiding moisture and touch contamination, and retiring them after five uses—help preserve performance and minimize risk.
Ultimately, the decision to reuse should weigh personal health status, exposure risk, and mask condition. When in doubt, err on the side of caution and replace the respirator. With thoughtful handling, your N95 can continue providing reliable protection across several uses—without sacrificing safety.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?