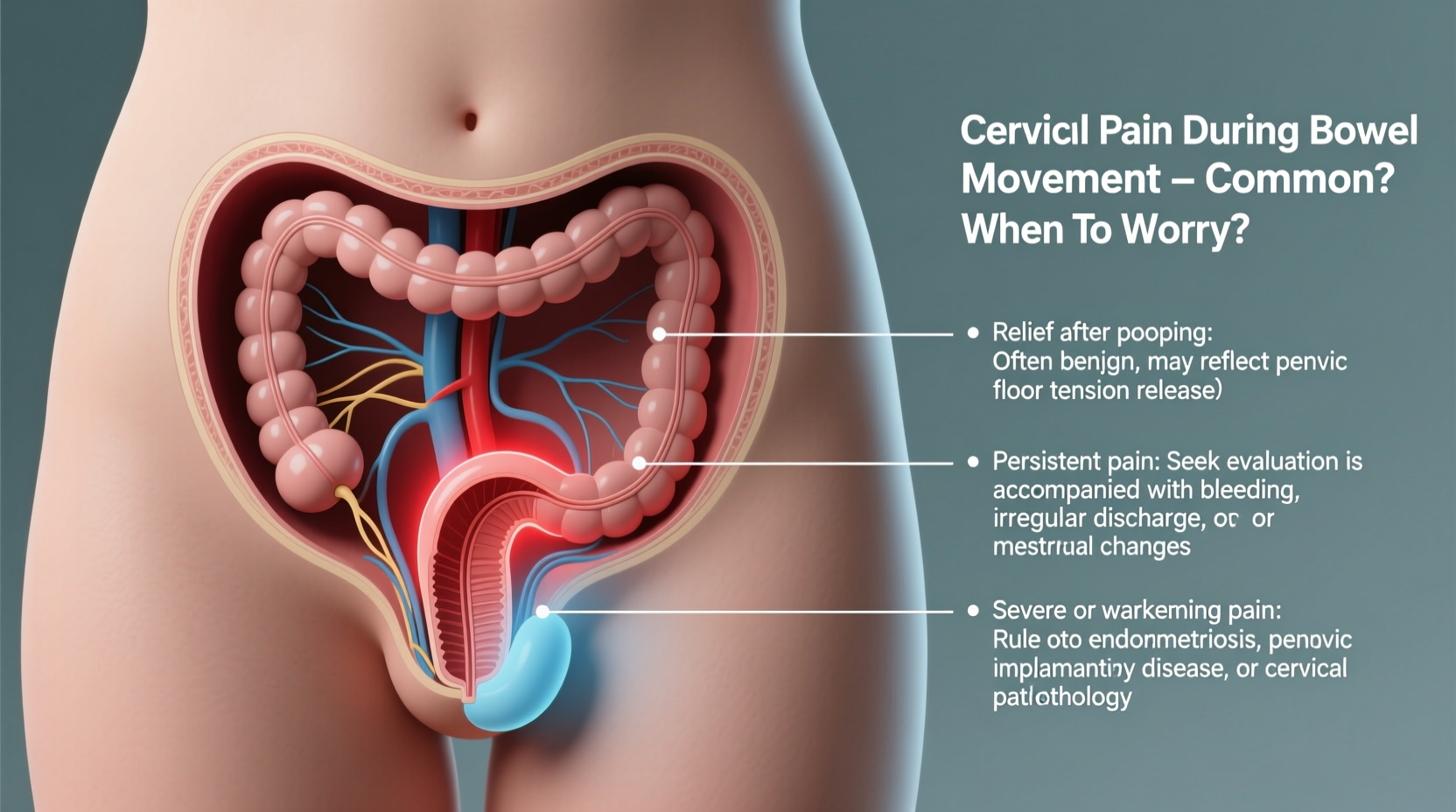
Experiencing cervix pain during bowel movements can be alarming and uncomfortable. While occasional discomfort may not signal a serious issue, persistent or severe pain warrants attention. The cervix, located at the lower end of the uterus, doesn’t directly interact with the bowels—but its proximity to the rectum and shared nerve pathways mean gastrointestinal activity can sometimes trigger referred pain. Understanding the underlying causes, effective relief methods, and red flags is essential for managing symptoms and knowing when to seek help.
Anatomy and Connection: Why Bowel Movements Affect Cervical Sensation
The pelvic region is densely packed with organs, nerves, and connective tissues. The cervix sits just above the vagina, anterior to the rectum. During defecation, pressure increases in the pelvic cavity. This pressure can indirectly affect the cervix—especially if inflammation, infection, or structural changes are present. Nerves from the rectum and cervix converge in the lower spine, so pain signals can be misinterpreted by the brain, leading to the sensation of cervical pain during bowel movements.
Additionally, conditions affecting nearby structures—such as the uterus, ovaries, or pelvic floor muscles—can refer pain to the cervix. For example, constipation-induced straining increases intra-abdominal pressure, which may compress sensitive tissues near the cervix, especially if adhesions or scar tissue exist from prior surgeries or infections.
Common Causes of Cervix Pain When Pooping
- Endometriosis: Tissue similar to the uterine lining grows outside the uterus, often on the cervix, rectum, or surrounding ligaments. During bowel movements, these lesions can become irritated, causing sharp or deep pain.
- Pelvic Inflammatory Disease (PID): An infection of the reproductive organs can lead to cervical tenderness. Straining may exacerbate this sensitivity.
- Cervical Erosion or Inflammation: Also known as ectropion, this condition exposes sensitive glandular cells on the cervix surface, making it more prone to irritation—even from indirect pressure.
- Uterine Fibroids: Noncancerous growths in the uterus can press against the cervix or rectum, especially if located posteriorly. Bowel movements may intensify this pressure.
- Pelvic Floor Dysfunction: Overactive or tight pelvic floor muscles can refer pain to the cervix. Straining during bowel movements worsens muscle tension.
- Constipation: Hard stools and excessive straining increase pressure on pelvic organs, potentially triggering referred cervical pain.
- Post-Surgical Adhesions: Scar tissue from procedures like cesarean sections or hysterectomies can bind organs together, causing pain with movement or pressure.
When to Worry: Red Flags Requiring Medical Evaluation
While mild discomfort may resolve with lifestyle adjustments, certain symptoms indicate the need for prompt medical care. These include:
- Severe or worsening pain during or after bowel movements
- Pain accompanied by fever, chills, or abnormal vaginal discharge
- Bleeding from the rectum or vagina unrelated to menstruation
- Pain that interferes with daily activities or sexual intercourse
- New or sudden onset of pain following surgery or infection
“Persistent cervix pain during defecation should never be dismissed as normal. It often points to an underlying gynecological or gastrointestinal condition that requires targeted treatment.” — Dr. Lena Patel, Gynecologist and Pelvic Pain Specialist
Relief Strategies and Home Management
For mild or intermittent cervix pain related to bowel movements, several self-care approaches can reduce discomfort:
Diet and Hydration
Maintaining soft stools minimizes straining. Increase fiber intake through fruits, vegetables, legumes, and whole grains. Drink at least 8–10 glasses of water daily. Consider a fiber supplement like psyllium husk if dietary changes aren’t sufficient.
Pelvic Floor Relaxation Techniques
Tension in the pelvic floor can amplify pain. Practice diaphragmatic breathing: inhale deeply through the nose, allowing the belly—and pelvic floor—to expand; exhale slowly. Repeat for 5–10 minutes daily. Warm baths can also relax tense muscles.
Proper Bowel Posture
Use a small footstool to elevate your feet while sitting on the toilet, creating a squat-like position. This aligns the rectum and reduces straining, decreasing pelvic pressure.
Over-the-Counter Support
Stool softeners (e.g., docusate sodium) or osmotic laxatives (e.g., polyethylene glycol) can prevent hard stools. Avoid stimulant laxatives long-term without medical guidance.
| Strategy | Action Step | Expected Benefit |
|---|---|---|
| Fiber Intake | Consume 25–30g daily from food or supplements | Softer stools, less straining |
| Hydration | Drink 2+ liters of water daily | Improved stool consistency |
| Toilet Posture | Use a footstool to raise knees above hips | Reduced pelvic strain |
| Heat Therapy | Apply heating pad to lower abdomen for 15–20 min | Muscle relaxation, pain reduction |
Medical Treatments Based on Diagnosis
Effective treatment depends on identifying the root cause. Diagnostic steps may include a pelvic exam, transvaginal ultrasound, or laparoscopy.
- For Endometriosis: Hormonal therapies (like birth control pills or GnRH agonists) can suppress lesion activity. Laparoscopic excision may be recommended for severe cases.
- For PID: Antibiotics are prescribed based on suspected pathogens. Early treatment prevents long-term complications like infertility.
- For Fibroids: Options range from medication (e.g., ulipristal acetate) to procedures like uterine artery embolization or myomectomy.
- For Pelvic Floor Dysfunction: Physical therapy with a certified pelvic floor therapist is highly effective. Biofeedback and manual therapy help retrain muscles.
Mini Case Study: Sarah’s Experience
Sarah, a 32-year-old teacher, began experiencing sharp pain in her cervix every time she had a bowel movement. Initially dismissing it as constipation, she noticed the pain persisted even after improving her diet. She also reported heavier periods and pain during sex. After a pelvic ultrasound and laparoscopy, she was diagnosed with deep infiltrating endometriosis affecting the uterosacral ligaments near the cervix. With hormonal treatment and pelvic floor therapy, her symptoms improved significantly within three months. Her case highlights the importance of not ignoring persistent pelvic pain—even if it seems linked to bowel function.
Step-by-Step Guide to Managing Cervix Pain During Bowel Movements
- Assess Symptoms: Note frequency, severity, and associated factors (menstrual cycle, sexual activity, bowel habits).
- Optimize Bowel Health: Increase fiber, hydrate well, and use proper toilet posture.
- Practice Pelvic Relaxation: Incorporate daily breathing exercises and warm baths.
- Track Progress: Keep a log for 2–4 weeks to evaluate improvement.
- Consult a Healthcare Provider: If pain persists beyond two weeks or worsens, schedule a gynecological evaluation.
- Follow Through on Testing: Complete recommended exams or imaging to identify underlying causes.
- Begin Targeted Treatment: Work with your provider on a plan tailored to your diagnosis.
FAQ
Can constipation really cause cervix pain?
Yes. Severe constipation increases pressure in the pelvic cavity. If the cervix is already sensitive due to inflammation, fibroids, or endometriosis, this pressure can trigger or worsen pain. Treating constipation often provides significant relief.
Is cervix pain during pooping a sign of cancer?
Rarely. While cervical cancer can cause pelvic pain, it typically presents with other symptoms like irregular bleeding, post-coital bleeding, or unusual discharge. Persistent pain should be evaluated, but it’s more commonly linked to benign conditions like endometriosis or fibroids.
Should I see a gastroenterologist or gynecologist?
Start with a gynecologist, as cervix-related pain is usually gynecological in origin. However, if bowel symptoms dominate—like chronic diarrhea, blood in stool, or weight loss—a gastroenterologist may also be needed.
Conclusion and Call to Action
Cervix pain when pooping is not something you should simply endure. While many causes are treatable and not life-threatening, ignoring the symptom can delay diagnosis of conditions like endometriosis or PID, which may impact fertility and quality of life. With the right combination of self-care, medical evaluation, and targeted treatment, most women find meaningful relief.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?