Waking up unable to breathe through your nose—or suddenly finding both nostrils completely blocked—can be more than just annoying. It disrupts sleep, affects concentration, and can make even simple daily tasks exhausting. While nasal congestion often seems minor, the inability to breathe freely impacts overall well-being. Understanding why both nostrils get blocked simultaneously and knowing how to address it effectively can bring quick relief and prevent recurring issues.
Why Both Nostrils Get Blocked at the Same Time
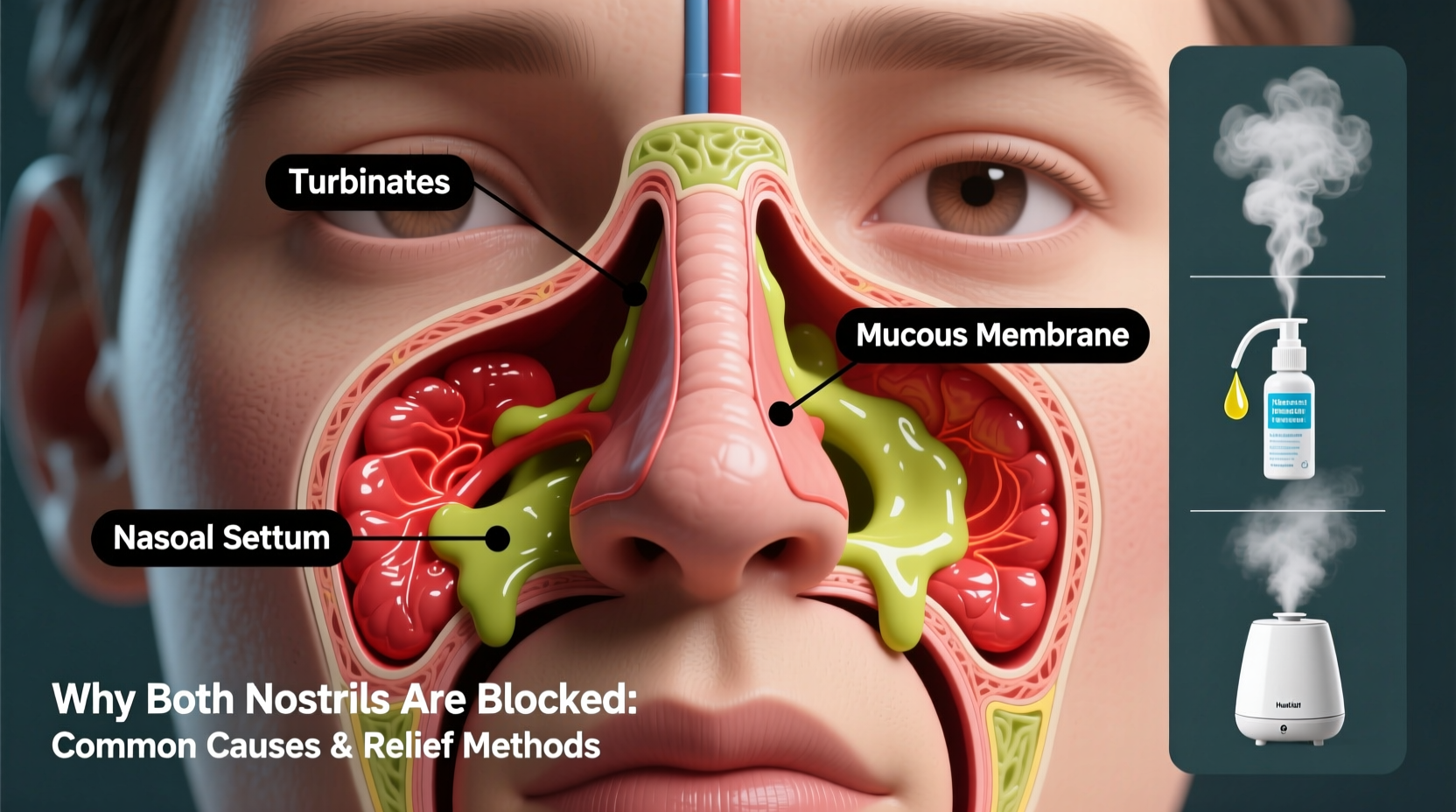
The human nasal cycle naturally alternates airflow between nostrils throughout the day. However, when both nostrils become congested at once, it’s typically due to inflammation or obstruction affecting the entire nasal passage. Common underlying causes include:
- Allergic rhinitis: Pollen, dust mites, pet dander, or mold trigger immune responses that cause widespread swelling in the nasal lining.
- Viral infections: Colds or flu lead to increased mucus production and inflamed tissues, often blocking both sides.
- Non-allergic rhinitis: Irritants like smoke, strong perfumes, temperature changes, or certain medications (e.g., blood pressure drugs) can induce bilateral congestion without an allergic component.
- Sinusitis: Infection or inflammation of the sinuses results in thick mucus buildup and pressure that blocks nasal passages symmetrically.
- Anatomical issues: A deviated septum may not always block one side completely but can reduce overall airflow capacity, making congestion feel worse on both sides during illness.
- Nasal polyps: Soft, noncancerous growths in the nasal passages or sinuses can obstruct airflow bilaterally when large or numerous.
“Bilateral nasal blockage is rarely due to structural problems alone. More often, it reflects systemic inflammation from infection, allergy, or environmental triggers.” — Dr. Lena Patel, Otolaryngologist
Effective Ways to Clear Clogged Nostrils
Relief depends on identifying the root cause, but several evidence-based methods work across multiple conditions. The goal is to reduce swelling, thin mucus, and restore normal airflow.
1. Saline Nasal Irrigation
Using a neti pot or saline spray flushes out allergens, bacteria, and excess mucus. Hypertonic saline solutions have been shown to improve drainage and decrease mucosal swelling faster than isotonic ones.
2. Steam Inhalation with Essential Oils
Inhaling warm, moist air helps loosen mucus. Adding eucalyptus or menthol oil may enhance decongestant effects by stimulating cold receptors in the nasal cavity, creating a sensation of improved airflow—even if actual congestion remains.
3. Humidify Your Environment
Dry indoor air aggravates nasal membranes. Using a cool-mist humidifier, especially at night, keeps mucus thin and reduces irritation. Aim for 40–60% humidity levels.
4. Over-the-Counter Medications
- Decongestants (pseudoephedrine, phenylephrine): Shrink swollen blood vessels in nasal tissue. Best for short-term use (3–5 days).
- Antihistamines (loratadine, cetirizine): Reduce allergic reactions causing congestion. May thicken mucus, so pair with hydration.
- Nasal corticosteroid sprays (fluticasone, budesonide): Decrease inflammation over time. Most effective for chronic allergies or polyps; take several days to reach full effect.
5. Hydration and Diet
Drinking plenty of fluids—especially warm liquids like herbal tea or broth—thins mucus. Avoid alcohol and caffeine, which can dehydrate and worsen congestion.
Step-by-Step Guide to Immediate Relief
Follow this timeline for rapid symptom reduction:
- Minute 0–5: Prepare a bowl of hot water with 2–3 drops of eucalyptus oil. Lean over it with a towel over your head and inhale deeply for 5 minutes.
- Minute 6–10: Perform a saline nasal rinse using a neti pot or squeeze bottle.
- Minute 11–15: Drink a cup of warm lemon water or ginger tea to stimulate circulation and mucus clearance.
- Hour 1: Apply a warm compress over the bridge of the nose and cheeks to ease sinus pressure.
- Next 24 hours: Use a humidifier while sleeping and consider taking an appropriate OTC medication based on suspected cause (allergy vs. infection).
Do’s and Don’ts When Dealing With Nasal Blockage
| Do’s | Don’ts |
|---|---|
| Use saline sprays regularly to moisturize nasal passages | Use decongestant nasal sprays for more than 3 consecutive days (risk of rebound congestion) |
| Stay hydrated with water and warm fluids | <Avoid smoking or exposure to secondhand smoke |
| Elevate your head while sleeping to promote drainage | Blow your nose too hard—this increases sinus pressure and risk of ear pain |
| Identify and remove allergens from your environment | Ignore persistent symptoms lasting more than 10 days—seek medical evaluation |
Real-Life Example: Managing Chronic Congestion
Sarah, a 34-year-old teacher, experienced constant bilateral nasal blockage every spring. She assumed it was “just allergies” and relied on antihistamines with limited success. After consulting an ENT specialist, she discovered she had both seasonal allergic rhinitis and small nasal polyps. Her treatment plan included daily fluticasone nasal spray, weekly saline irrigation, and allergen-proof bedding. Within six weeks, her nighttime breathing improved dramatically, and daytime fatigue decreased. This case illustrates how overlapping conditions can amplify symptoms and why targeted diagnosis matters.
When to See a Doctor
Most cases of nasal congestion resolve within a week. However, seek medical attention if you experience any of the following:
- Facial pain or swelling lasting more than a week
- Thick yellow-green discharge with fever (signs of bacterial sinusitis)
- Loss of smell for more than 10 days
- Recurrent episodes suggesting polyps or structural issues
- Congestion disrupting sleep or daily function despite home care
An otolaryngologist (ENT) can perform nasal endoscopy or imaging to identify polyps, septal deviation, or chronic sinus disease requiring specialized treatment.
Frequently Asked Questions
Why do I only get both nostrils blocked at night?
Lying down increases blood flow to the nasal area, exacerbating swelling. Additionally, indoor allergens like dust mites in pillows or low humidity from heating systems can worsen nighttime congestion.
Can acid reflux cause nasal blockage?
Yes. Laryngopharyngeal reflux (silent reflux) can irritate the upper airway and contribute to postnasal drip and chronic congestion, even without heartburn symptoms.
Is it safe to use nasal strips every night?
Nasal strips are generally safe for nightly use. They mechanically open the nasal passages and can improve airflow during sleep, especially for those with mild obstruction or snoring.
Take Control of Your Breathing
Breathing should be effortless. Persistent bilateral nasal blockage isn’t something to ignore or endure long-term. Whether triggered by allergies, infection, or anatomical factors, effective solutions exist. Start with gentle, consistent measures like saline rinses and humidity control. Track your symptoms and response to treatments. If congestion persists, don’t hesitate to consult a healthcare provider for a precise diagnosis. Small changes in daily habits can lead to significant improvements in breathing, sleep quality, and overall health.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?