Throughout the pandemic, a puzzling phenomenon has emerged: some individuals remain completely unscathed by SARS-CoV-2, even after repeated exposure. Living with infected family members, working in high-risk environments, or traveling during surges—yet never testing positive or showing symptoms. This isn’t just luck. A growing body of research suggests that biological, genetic, and immunological factors play a crucial role in determining who gets sick and who doesn’t. Understanding these mechanisms offers not only personal insight but also critical clues for future treatments and public health strategies.
The Role of Pre-Existing Immunity
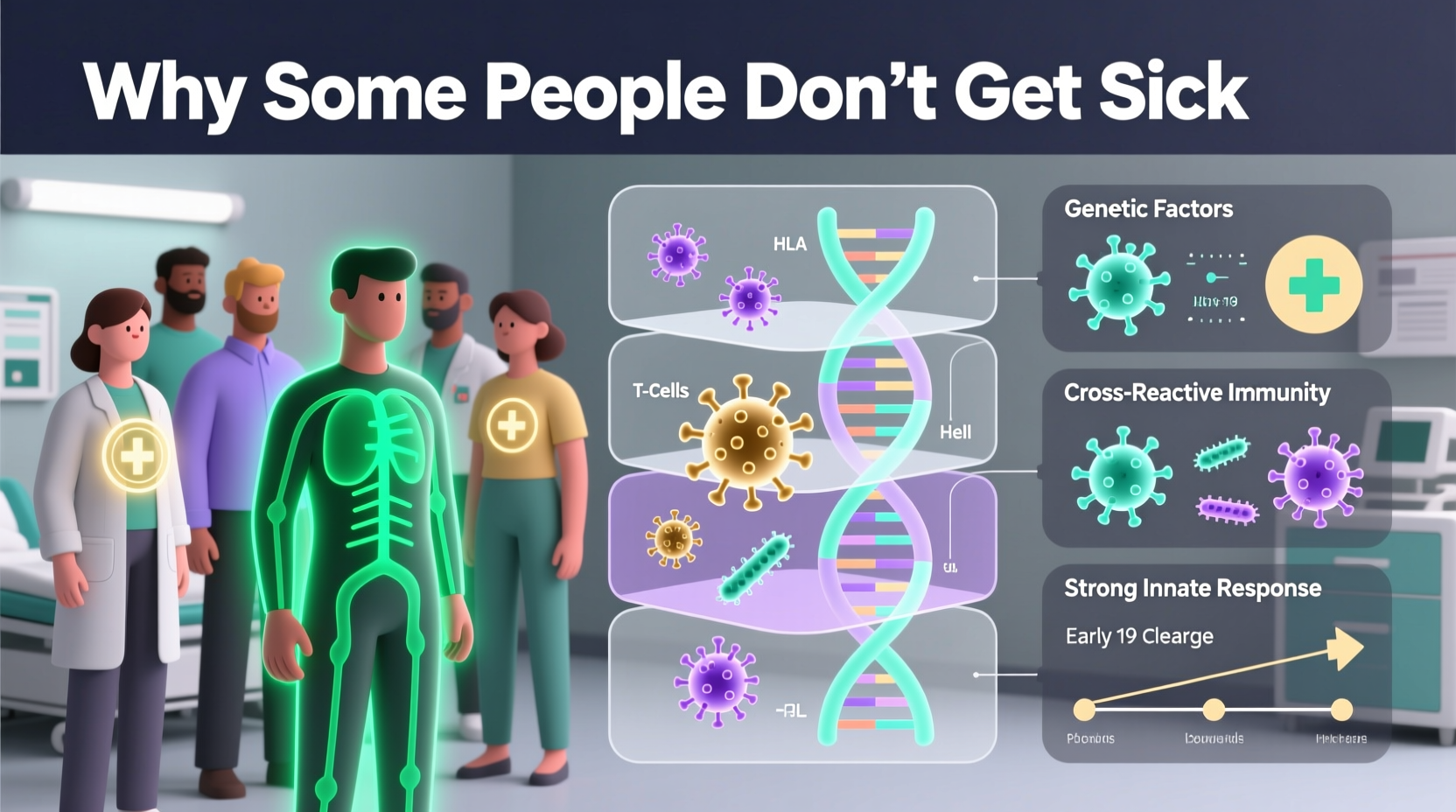
One of the most compelling explanations for resistance to COVID-19 lies in pre-existing immunity. Some individuals possess immune cells capable of recognizing SARS-CoV-2 due to prior exposure to other coronaviruses—common colds caused by related viruses like HCoV-OC43 or HCoV-229E.
T-cells, particularly CD4+ and CD8+ T-cells, are central to this cross-reactive defense. Studies conducted at the La Jolla Institute for Immunology found that up to 50% of people tested had T-cells that reacted to SARS-CoV-2 despite no prior exposure to it. These memory T-cells likely originated from past encounters with seasonal coronaviruses.
This cross-protection doesn’t always prevent infection but can significantly reduce viral load and symptom severity—sometimes resulting in asymptomatic cases mistaken for full resistance.
Genetic Factors That Influence Resistance
Genetics may be one of the strongest determinants of why some people never get sick. Scientists have identified specific gene variants associated with reduced susceptibility to SARS-CoV-2.
A landmark study published in Nature in 2021 revealed that individuals carrying a rare mutation in the IFNAR2 gene—involved in interferon signaling—were nearly 10 times more likely to resist symptomatic infection. Interferons are proteins that act as first responders in viral defense, triggering antiviral activity in neighboring cells.
Another key player is the HLA (human leukocyte antigen) system, which helps the immune system distinguish between self and non-self proteins. Specific HLA types, such as HLA-B*15:01, have been linked to asymptomatic infection. People with this variant can mount a rapid immune response without ever feeling ill.
“Some individuals are genetically wired to detect and eliminate the virus before it establishes a foothold.” — Dr. Mary Carrington, National Cancer Institute, Immunogenetics Researcher
Resilient Mucosal Immunity and Nasal Defenses
The first line of defense against respiratory viruses is not the bloodstream—it’s the mucosal lining of the nose and throat. Recent research highlights the importance of innate immune responses in nasal epithelial cells.
A 2023 study from University College London found that people who remained uninfected despite household exposure produced higher levels of antiviral interferons in their nasal passages within hours of viral contact. Their cells acted like sentinels, shutting down viral replication before it could spread.
This early warning system appears to be influenced by both genetics and environmental conditioning—such as previous viral exposures or even lifestyle factors like diet and sleep.
Key Components of Nasal Immune Defense
- Rapid interferon release upon detection of viral RNA
- Dense populations of resident memory T-cells in upper airways
- Mucus with high concentrations of IgA antibodies
- Presence of commensal microbes that modulate immune tone
Behavioral and Environmental Influences
While biology plays a major role, behavior cannot be ignored. Even among those with favorable genetics, consistent protective habits amplify resistance.
Consider two individuals with identical genetic profiles: one maintains good sleep hygiene, manages stress, eats a nutrient-rich diet, and avoids crowded indoor spaces; the other works night shifts, smokes, and frequently attends large gatherings. The former is far more likely to avoid infection—not solely due to genes, but because their immune system operates at peak efficiency.
| Factor | Supports Resistance? | Scientific Evidence Level |
|---|---|---|
| Vitamin D sufficiency | Yes | Strong observational, moderate clinical |
| Regular physical activity | Yes | Strong |
| Chronic stress | No | Well-documented immunosuppressive effect |
| Sleep deprivation | No | Proven to reduce T-cell function |
| Frequent handwashing | Yes | Epidemiologically supported |
Mini Case Study: The Healthcare Worker Who Never Tested Positive
Jamila R., a nurse in New York City, worked throughout the 2020–2021 surge in an ICU treating critically ill COVID-19 patients. Despite inconsistent access to N95 masks during early shortages and living with a partner who contracted the virus, Jamila never developed symptoms or tested positive—even when routinely screened.
When enrolled in a research study at Rockefeller University, her blood showed robust cross-reactive T-cell responses and elevated baseline interferon-stimulated gene expression. Genetic testing revealed she carried the HLA-B*15:01 allele and a favorable variant in the OAS1 gene, both linked to rapid viral clearance. Her case exemplifies how genetics, prior immune training, and disciplined hygiene can combine to confer near-complete resistance.
Step-by-Step: How You Can Strengthen Your Natural Defenses
While you can’t change your genes, you can optimize the environment in which your immune system operates. Follow this science-backed timeline to enhance your resilience:
- Week 1–2: Assess & Adjust Lifestyle
- Track sleep (aim for 7–8 hours)
- Eliminate smoking and excessive alcohol
- Begin daily 30-minute walks
- Week 3–4: Optimize Nutrition
- Incorporate zinc-rich foods (pumpkin seeds, legumes)
- Increase vitamin C (citrus, bell peppers)
- Add fermented foods for gut microbiome support
- Month 2: Monitor Biomarkers
- Check vitamin D levels via blood test
- Consider hs-CRP to assess inflammation
- Discuss immune panel with physician if recurrent infections occur
- Ongoing: Maintain Immune Fitness
- Practice stress-reduction techniques (mindfulness, breathing)
- Stay current on vaccinations (including updated boosters)
- Wash hands regularly and ventilate indoor spaces
FAQ: Common Questions About COVID-19 Resistance
Can someone be naturally immune to all variants of SARS-CoV-2?
Complete immunity to all variants is unlikely, but certain genetic and immunological profiles offer broad protection across multiple strains. Cross-reactive T-cells and strong mucosal responses may provide durable defense, though new variants with immune escape mutations can still pose risks.
Does having had many colds make me more resistant?
Possibly. Repeated exposure to seasonal coronaviruses may train your T-cells to respond faster to SARS-CoV-2. However, this does not guarantee protection—especially in older adults or those with compromised immunity.
If I’ve never gotten COVID, should I still get vaccinated?
Yes. Vaccination enhances existing immunity and provides more consistent, measurable protection. Natural resistance mechanisms vary and may not hold against future variants. Vaccines add a reliable layer of defense.
Conclusion: Harnessing the Science of Resilience
The mystery of why some people don’t get sick from COVID-19 is unraveling through advances in immunology and genetics. While a fortunate few benefit from rare gene variants or potent cross-immunity, everyone can take meaningful steps to strengthen their body’s defenses. The goal isn’t just to avoid one virus—it’s to build a resilient immune system capable of handling future threats.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?