Stool color is a reliable indicator of digestive health. While brown is normal, changes—especially dark or black stools—can signal underlying conditions. Most cases are harmless, linked to diet or medication, but some point to serious gastrointestinal issues. Understanding the difference between benign causes and warning signs helps you decide when to consult a doctor.
What Causes Dark Poop?
Stool color results from bile—a liver-produced fluid that aids fat digestion—and its interaction with gut bacteria. As bile breaks down, it turns stool from green to various shades of brown. Deviations from this norm can result in darker-than-usual feces.
The most common causes of dark poop include:
- Dietary factors: Foods like black licorice, blueberries, beets, and iron-rich meals may darken stool.
- Medications and supplements: Iron supplements, bismuth subsalicylate (Pepto-Bismol), and certain antibiotics alter stool color.
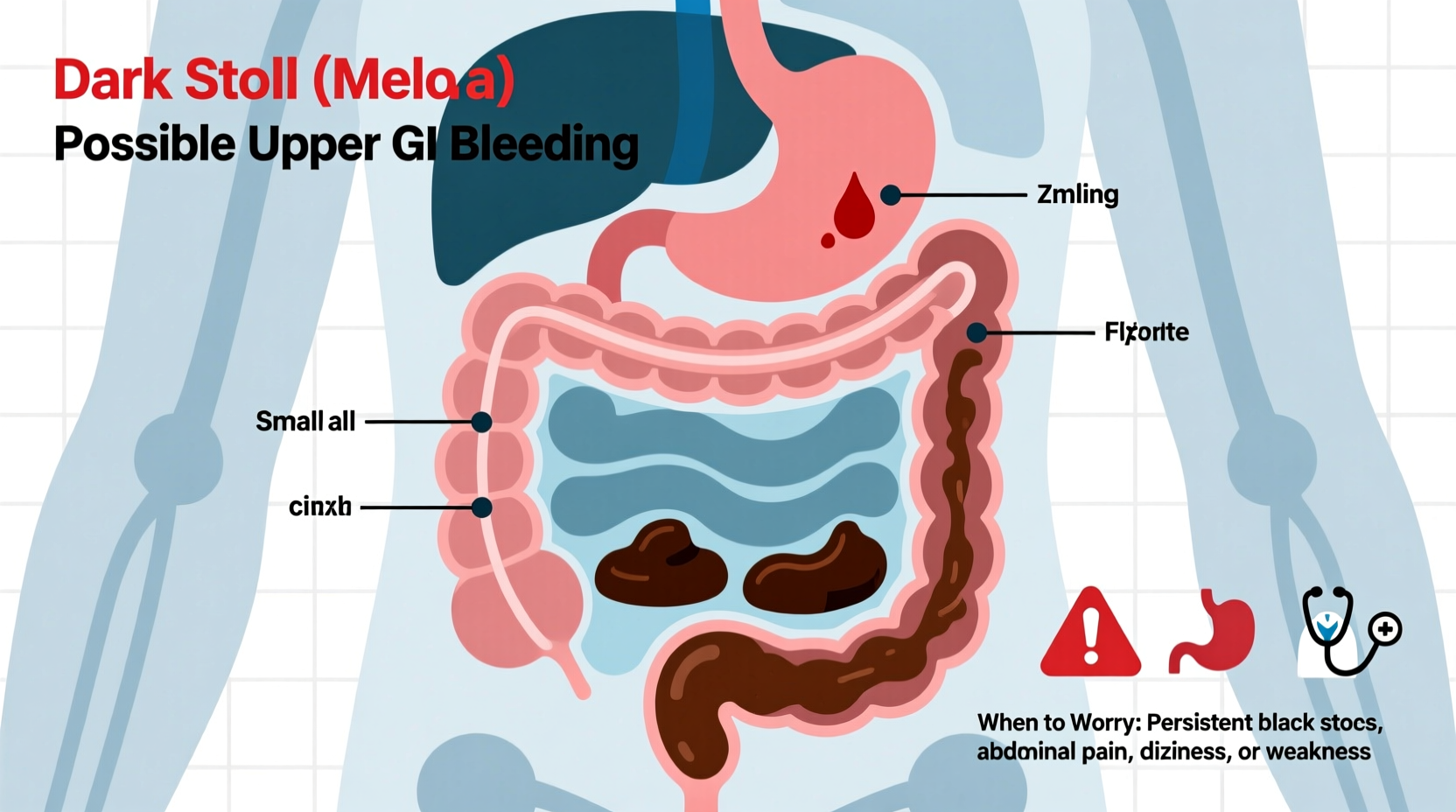
- Gastrointestinal bleeding: Blood from the upper digestive tract (stomach, esophagus, small intestine) oxidizes as it moves through the intestines, turning stool black and tarry—a condition known as melena.
- Liver disease: Cirrhosis or bile duct obstruction can disrupt normal bile flow, affecting stool pigmentation.
- Ulcers or gastritis: Chronic inflammation or sores in the stomach lining may cause slow bleeding.
Melena vs. Pseudomelena: Understanding the Difference
Not all black stools indicate internal bleeding. The distinction lies in whether the discoloration comes from blood (melena) or external sources (pseudomelena).
| Feature | Melena (True) | Pseudomelena (False) |
|---|---|---|
| Appearance | Black, sticky, tar-like | Dull black or speckled |
| Odor | Foul, distinctive “rotten” smell | Normal or slightly altered |
| Cause | Upper GI bleeding (e.g., ulcer, varices) | Food, supplements, medications |
| Consistency | Thick, glossy | Normal or slightly firm |
| Wipes after flushing | Leaves dark smears that don’t wipe clean | Color washes off easily |
If your stool resembles tar, has a strong odor, and doesn’t rinse away cleanly, melena is likely. This requires prompt evaluation.
“Black, tarry stools with a foul smell should never be ignored. They often indicate significant upper GI bleeding.” — Dr. Lena Torres, Gastroenterologist at Boston Medical Center
When to Worry: Red Flags That Demand Medical Attention
Occasional dark stool without other symptoms is usually not concerning. However, certain signs suggest an urgent need for medical care:
- Sudden onset of black, sticky, foul-smelling stool
- Dizziness, lightheadedness, or fainting
- Vomiting blood or material resembling coffee grounds
- Abdominal pain or cramping
- Unexplained weight loss
- Persistent fatigue or shortness of breath (signs of anemia)
- History of peptic ulcers, liver disease, or alcohol abuse
These symptoms, especially in combination, may point to serious conditions such as gastric ulcers, esophageal varices, Mallory-Weiss tears, or even stomach cancer.
Case Example: Recognizing a Silent Bleed
James, a 54-year-old office worker, noticed his stool had turned jet black over three days. He dismissed it initially, attributing it to his new multivitamin. But when he began feeling unusually tired and lightheaded during meetings, he visited his doctor. Blood tests revealed severe iron-deficiency anemia. An endoscopy uncovered a bleeding duodenal ulcer. Early intervention stopped the bleed and prevented hospitalization. James’s case illustrates how subtle symptoms can mask serious internal bleeding.
Diagnostic Steps and What to Expect
If you present with persistent dark stools and concerning symptoms, your doctor will likely follow a structured diagnostic path:
- Medical history review: Questions about diet, medications, alcohol use, and prior GI issues.
- Physical exam: Checking for abdominal tenderness, enlarged liver, or signs of anemia.
- Stool test: A fecal occult blood test (FOBT) detects hidden blood.
- Blood work: To check hemoglobin levels and assess for anemia.
- Endoscopy: A camera-equipped tube examines the esophagus, stomach, and upper intestine. This is the gold standard for identifying bleeding sources.
- Imaging: CT scans or capsule endoscopy if the source isn’t found via traditional scope.
Treatment depends on the diagnosis. Ulcers may be treated with proton pump inhibitors and antibiotics (if H. pylori is present). Varices require banding or medication to reduce portal pressure. In emergencies, blood transfusions or surgery may be necessary.
Prevention and Lifestyle Adjustments
You can reduce the risk of developing conditions that lead to dark, bloody stools by adopting healthier habits:
- Avoid excessive alcohol consumption, which damages the stomach lining and liver.
- Limits use of NSAIDs; opt for acetaminophen when possible.
- Eat a balanced diet rich in fiber to support digestive health.
- Manage stress, as it can exacerbate acid production and ulcers.
- Get screened for H. pylori if you have recurrent stomach pain.
“Many patients don’t realize that chronic ibuprofen use can silently erode the stomach lining. Prevention starts with awareness.” — Dr. Arjun Patel, Internal Medicine Specialist
FAQ
Can eating blueberries turn my poop black?
Yes, large quantities of blueberries or blackberries can temporarily darken stool. Unlike melena, the stool won’t be sticky or foul-smelling, and the effect resolves within a day or two.
I take iron supplements and have dark stools. Should I stop?
Iron commonly causes dark or black stools—it’s a known side effect, not a sign of bleeding. Do not stop taking prescribed iron without consulting your doctor, especially if you’re being treated for anemia.
Is dark poop always a sign of cancer?
No. While gastrointestinal cancers can cause melena, they are less common causes. More often, ulcers, medication, or diet are responsible. However, unexplained dark stools in people over 50 should be evaluated to rule out malignancy.
Action Checklist: What to Do If You Notice Dark Stools
- Review recent diet: Did you eat dark-colored foods or take iron/Pepto-Bismol?
- Note consistency and smell: Is it tarry and foul? Could it be melena?
- Check for additional symptoms: Fatigue, dizziness, abdominal pain, vomiting?
- Stop unnecessary NSAIDs and alcohol temporarily.
- Contact your healthcare provider if symptoms persist beyond 48 hours or red flags appear.
- Prepare for possible testing: Bring a list of medications and symptoms to your appointment.
Conclusion
Dark poop isn’t always dangerous, but it shouldn’t be ignored when accompanied by other symptoms. Your body uses stool color as a signal—learning to interpret it empowers you to act early. Whether it's adjusting your diet, reevaluating medications, or seeking timely medical care, proactive steps protect your long-term digestive health. Don’t wait for symptoms to worsen. Pay attention, respond wisely, and consult a professional when in doubt.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?