Waking up with a sudden spinning sensation or feeling unsteady when turning in bed is more than just disorienting—it can disrupt sleep, affect balance, and raise concerns about underlying health. This form of dizziness, often triggered by changes in head position, is commonly experienced but not always well understood. While occasional lightheadedness may be harmless, recurring vertigo when lying down warrants attention. Understanding the root causes, recognizing key symptoms, and knowing how to respond can make a significant difference in managing this condition effectively.
Understanding Positional Dizziness: Why It Happens
Dizziness when lying down is frequently linked to issues within the inner ear—the body’s primary balance center. The vestibular system detects motion and spatial orientation. When tiny calcium crystals (otoconia) in the inner ear become dislodged, they can enter the semicircular canals and send false signals to the brain about movement, resulting in vertigo. This phenomenon is most commonly associated with benign paroxysmal positional vertigo (BPPV), the leading cause of positional dizziness.
BPPV episodes are typically brief—lasting less than a minute—but intense. They occur predictably with specific movements: rolling over in bed, tilting the head back, or getting up from a lying position. Unlike general lightheadedness caused by low blood pressure or dehydration, BPPV produces a distinct spinning sensation known as vertigo.
“Positional vertigo is one of the most treatable forms of dizziness, yet it's often misdiagnosed or ignored.” — Dr. Lena Torres, Neurotologist
Common Causes of Dizziness When Lying Down
While BPPV is the top culprit, several other conditions can trigger dizziness upon reclining or shifting positions:
- Benign Paroxysmal Positional Vertigo (BPPV): Displaced inner ear crystals cause brief but intense vertigo.
- Vestibular Neuritis: Inflammation of the vestibular nerve, often following a viral infection, leads to prolonged dizziness without hearing loss.
- Ménière’s Disease: A disorder involving fluid buildup in the inner ear, causing vertigo, tinnitus, and hearing fluctuations—sometimes worsened by lying flat.
- Cervicogenic Dizziness: Neck stiffness or injury can interfere with proprioceptive signals, affecting balance during position changes.
- Orthostatic Hypotension: A sudden drop in blood pressure when changing posture, including lying down or sitting up, may cause lightheadedness.
- Anxiety or Hyperventilation: Rapid breathing or panic attacks can alter blood CO₂ levels, inducing dizziness that feels worse at night.
- Medication Side Effects: Certain antihypertensives, sedatives, or antidepressants may impair balance regulation.
Symptoms That Signal When to Seek Help
Not all dizziness requires emergency care, but certain red flags indicate the need for prompt medical evaluation:
| Symptom | May Indicate | Action |
|---|---|---|
| Spinning sensation lasting >1 minute | Persistent BPPV or central vertigo | See an ENT or neurologist |
| Nausea or vomiting with dizziness | Vestibular dysfunction | Monitor frequency; consult if recurrent |
| Hearing loss or ringing in ears | Ménière’s disease or acoustic neuroma | Immediate audiology referral |
| Double vision, slurred speech, or weakness | Possible stroke or neurological issue | Seek emergency care |
| Dizziness upon standing AND lying | Blood pressure dysregulation | Check BP at different positions |
If dizziness is accompanied by chest pain, fainting, confusion, or difficulty walking, seek urgent medical attention. These could point to cardiovascular or central nervous system disorders.
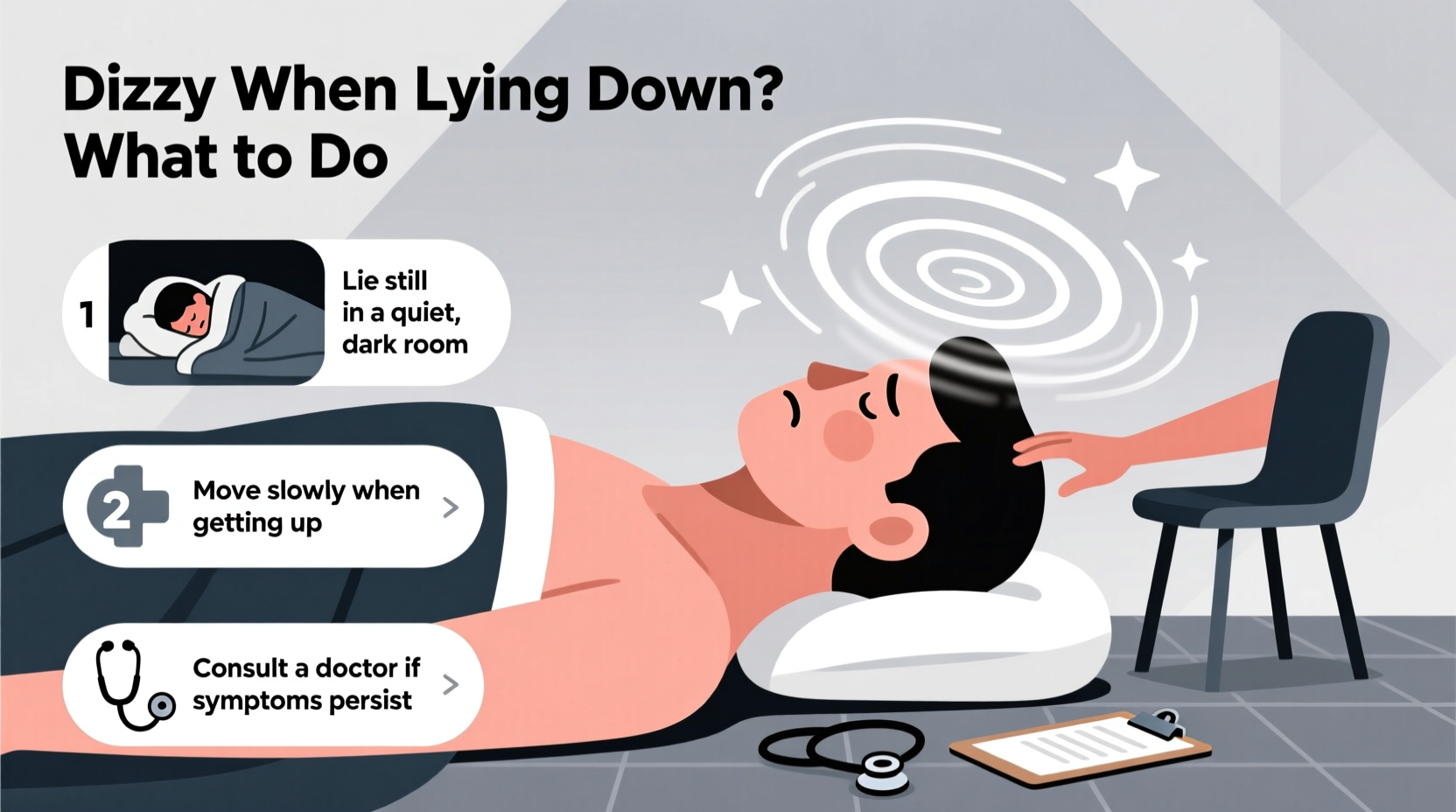
Step-by-Step Guide to Managing Dizziness at Bedtime
For those experiencing recurring vertigo when lying down, especially due to BPPV, a structured approach can bring rapid relief:
- Confirm the Pattern: Note whether dizziness happens only when rolling to one side or both. Most BPPV cases affect one ear and one direction.
- Avoid Sudden Movements: Move slowly when transitioning from sitting to lying. Use your arms to pivot gently.
- Try the Epley Maneuver: A series of head movements designed to reposition loose crystals in the inner ear. Best performed under guidance initially.
- Elevate Your Head: Sleep with two pillows or use a wedge pillow to reduce fluid shifts and minimize positional triggers.
- Limit Caffeine and Salt: Especially important if Ménière’s is suspected, as these can increase inner ear fluid pressure.
- Stay Hydrated: Dehydration affects blood volume and electrolyte balance, potentially worsening dizziness.
- Review Medications: Consult your doctor about drugs that might contribute to imbalance.
Mini Case Study: Resolving Nighttime Vertigo
Sarah, a 54-year-old teacher, began experiencing sharp vertigo every time she turned onto her right side in bed. The room would spin for about 30 seconds, making it hard to fall asleep. After ruling out neurological issues, her ENT diagnosed right-sided posterior canal BPPV. She was shown the Epley maneuver during her visit. Performing it at home twice daily for three days, her symptoms resolved completely. Six months later, with no recurrence, she credits early intervention and proper technique for her recovery.
Practical Tips and Prevention Checklist
Use this checklist to manage and prevent positional dizziness:
- ✅ Learn and practice the Epley maneuver if diagnosed with BPPV
- ✅ Avoid sleeping flat—use a wedge pillow or extra support
- ✅ Turn onto your non-affected side first when rolling in bed
- ✅ Stay hydrated throughout the day, especially in warm climates
- ✅ Reduce intake of salt, alcohol, and caffeine
- ✅ Address neck tension with gentle stretches or physical therapy
- ✅ Schedule regular checkups if you have a history of vertigo
Frequently Asked Questions
Can dehydration cause dizziness when lying down?
Yes. Dehydration reduces blood volume, which can lead to orthostatic hypotension—a drop in blood pressure when changing positions. Even lying down after being upright can trigger lightheadedness if hydration is poor. Maintaining consistent fluid intake helps stabilize circulation and supports inner ear function.
Is it normal to feel dizzy every time I lie on my back?
No, persistent dizziness in any position is not normal. If lying flat consistently causes vertigo, it may indicate BPPV affecting the posterior canal or another vestibular disorder. Chronic symptoms should be evaluated by a healthcare provider to rule out structural or neurological causes.
How long does BPPV usually last without treatment?
Untreated BPPV can persist for weeks or even months, though some cases resolve spontaneously within a few weeks. However, targeted treatments like the Epley maneuver often provide relief in just 1–3 sessions. Delaying treatment increases the risk of falls and impacts quality of life unnecessarily.
Take Control of Your Balance and Comfort
Dizziness when lying down is a common but manageable condition. With accurate diagnosis and simple, evidence-based interventions, most people regain full stability and restful sleep. Ignoring symptoms or assuming they’ll disappear on their own can prolong discomfort and increase fall risk, especially in older adults. Whether through self-administered maneuvers, lifestyle adjustments, or professional care, taking proactive steps makes a tangible difference.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?