Standing up from a seated or lying position should be a seamless motion. But if you frequently feel lightheaded, unsteady, or like the room is spinning when you rise, you're not alone. This sensation—often described as dizziness upon standing—is medically known as orthostatic hypotension or postural hypotension. While occasional mild dizziness may be harmless, recurring or severe episodes can signal underlying health issues. Understanding the causes, knowing how to respond, and recognizing warning signs can help prevent falls and serious complications.
What Happens When You Get Dizzy Upon Standing?
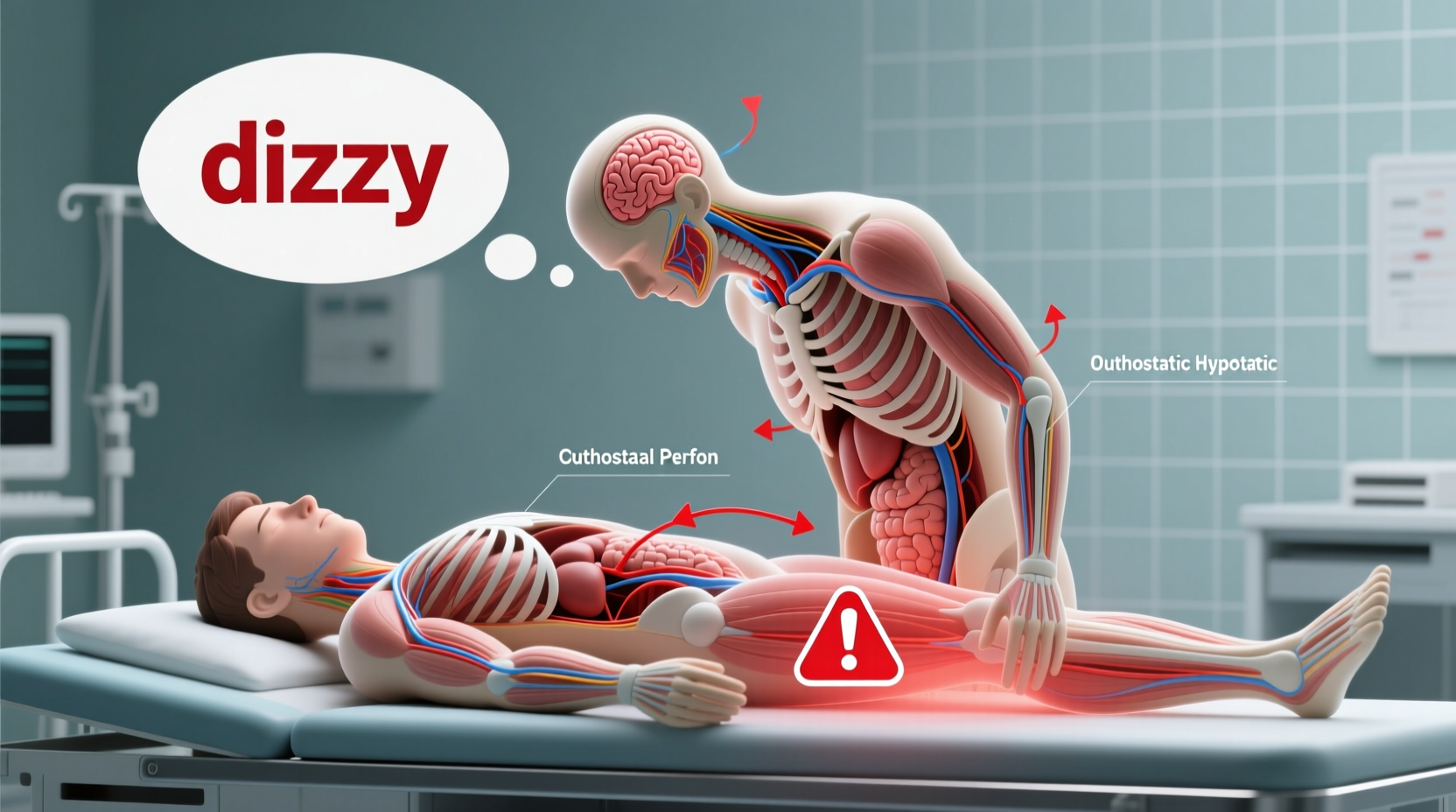
When you stand up, gravity pulls blood downward into your legs and abdomen. Normally, your body compensates by increasing heart rate and constricting blood vessels to maintain steady blood flow to the brain. If this system falters, blood pressure drops suddenly, leading to reduced cerebral perfusion. This temporary lack of oxygen to the brain causes symptoms such as:
- Lightheadedness or faintness
- Blurred vision
- Nausea
- Weakness
- Trouble concentrating
- Feeling like you might pass out
The duration of symptoms varies. Most people experience relief within seconds, but some may feel off-balance for minutes. Persistent or worsening dizziness requires attention.
Common Causes of Dizziness When Standing Up
Dizziness upon standing isn't a condition in itself—it's a symptom. The root cause can range from benign to serious. Common contributors include:
Dehydration
Inadequate fluid intake reduces blood volume, making it harder for the body to regulate blood pressure. This is especially common in hot weather, after exercise, or during illness.
Medications
Several drugs can lower blood pressure or interfere with autonomic regulation. These include:
- Diuretics (water pills)
- Alpha-blockers for prostate or hypertension
- Antidepressants (especially tricyclics)
- Heart medications like beta-blockers or nitrates
- Parkinson’s disease treatments
Age-Related Changes
As we age, the body’s ability to regulate blood pressure declines. Blood vessels become less elastic, and the autonomic nervous system slows its response time. People over 65 are at higher risk.
Prolonged Bed Rest or Inactivity
Extended periods of sitting or lying down—such as during recovery from surgery—can impair circulatory adaptation. Even sitting through long flights may trigger transient dizziness.
Medical Conditions
Certain chronic illnesses disrupt normal blood pressure control:
- Diabetes: Can damage nerves involved in blood pressure regulation (autonomic neuropathy).
- Parkinson’s disease: Affects autonomic function and dopamine-related blood pressure control.
- Heart conditions: Arrhythmias, heart failure, or valve problems reduce cardiac output.
- Anemia: Low red blood cell count decreases oxygen delivery, amplifying dizziness.
- Adrenal insufficiency: Impacts hormone regulation of blood pressure.
“Orthostatic hypotension is more than just a nuisance—it’s a window into cardiovascular and neurological health.” — Dr. Linda Chen, Neurologist and Autonomic Specialist
What to Do When You Feel Dizzy Standing Up
If you feel lightheaded upon standing, act quickly to prevent injury. Follow these steps:
- Stop and hold on: Grab a stable surface like a wall, chair, or counter to avoid falling.
- Bend forward or sit down: Lowering your head below heart level increases blood flow to the brain.
- Wait it out: Stay still until the dizziness passes, usually within 10–30 seconds.
- Stand slowly: After lying down, move in stages—lie to sit, sit to stand—with pauses between.
- Stay hydrated: Sip water throughout the day, especially in warm environments.
When to Worry: Red Flags That Need Medical Attention
Occasional, brief dizziness is usually not dangerous. However, certain symptoms suggest a need for prompt evaluation:
| Symptom | Why It’s Concerning |
|---|---|
| Fainting (syncope) | Could indicate heart rhythm issues or severe autonomic dysfunction |
| Chest pain or palpitations | May signal arrhythmia or heart disease |
| Shortness of breath | Possible heart or lung problem affecting oxygen supply |
| Confusion or slurred speech | Could point to stroke or neurological event |
| Dizziness lasting more than a few minutes | Suggests inadequate compensation; may require treatment |
Also seek help if dizziness happens daily, interferes with activities, or begins suddenly after starting a new medication.
Mini Case Study: Recognizing a Silent Issue
John, a 72-year-old retiree, began noticing he felt “woozy” every morning when getting out of bed. He dismissed it as aging, but one day he fainted while brushing his teeth. His daughter urged him to see a doctor. Tests revealed low blood volume due to a diuretic he’d been taking for high blood pressure. His dose was adjusted, and he was advised to increase salt and fluid intake. Within a week, his symptoms improved dramatically. John’s case shows how a simple medication adjustment, prompted by awareness, can prevent serious falls.
Prevention and Long-Term Management Checklist
Managing dizziness when standing up often involves lifestyle changes and medical oversight. Use this checklist to stay proactive:
- ✅ Drink 6–8 glasses of water daily unless restricted by a doctor
- ✅ Rise slowly from sitting or lying positions
- ✅ Avoid prolonged standing, especially in hot environments
- ✅ Review all medications with your doctor annually
- ✅ Eat smaller, more frequent meals to prevent postprandial drops in blood pressure
- ✅ Wear compression stockings if recommended by a physician
- ✅ Monitor blood pressure at home, especially when symptomatic
- ✅ Exercise regularly to improve circulation and vascular tone
Frequently Asked Questions
Can low iron cause dizziness when standing up?
Yes. Iron deficiency anemia reduces the blood’s oxygen-carrying capacity. When combined with positional changes, this can intensify lightheadedness. Fatigue, pale skin, and shortness of breath are other common signs.
Is it normal to feel dizzy after eating?
Some people experience postprandial hypotension—low blood pressure after meals—especially older adults. Blood diverts to the digestive tract, reducing supply elsewhere. Eating smaller, low-carbohydrate meals can help minimize this effect.
Can anxiety cause dizziness when standing?
Anxiety can mimic or worsen dizziness, but it typically doesn’t cause true orthostatic hypotension. However, hyperventilation during anxiety attacks may lead to lightheadedness that feels similar. A proper diagnosis requires measuring blood pressure and heart rate in different positions.
Conclusion: Take Control of Your Stability
Dizziness when standing up is more than just a minor inconvenience—it can be a clue to deeper health dynamics. While many cases resolve with hydration, slower movements, and medication adjustments, ignoring persistent symptoms risks falls, injuries, and missed diagnoses. By understanding your body’s signals, applying practical strategies, and knowing when to consult a healthcare provider, you can regain confidence in your balance and overall well-being.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?