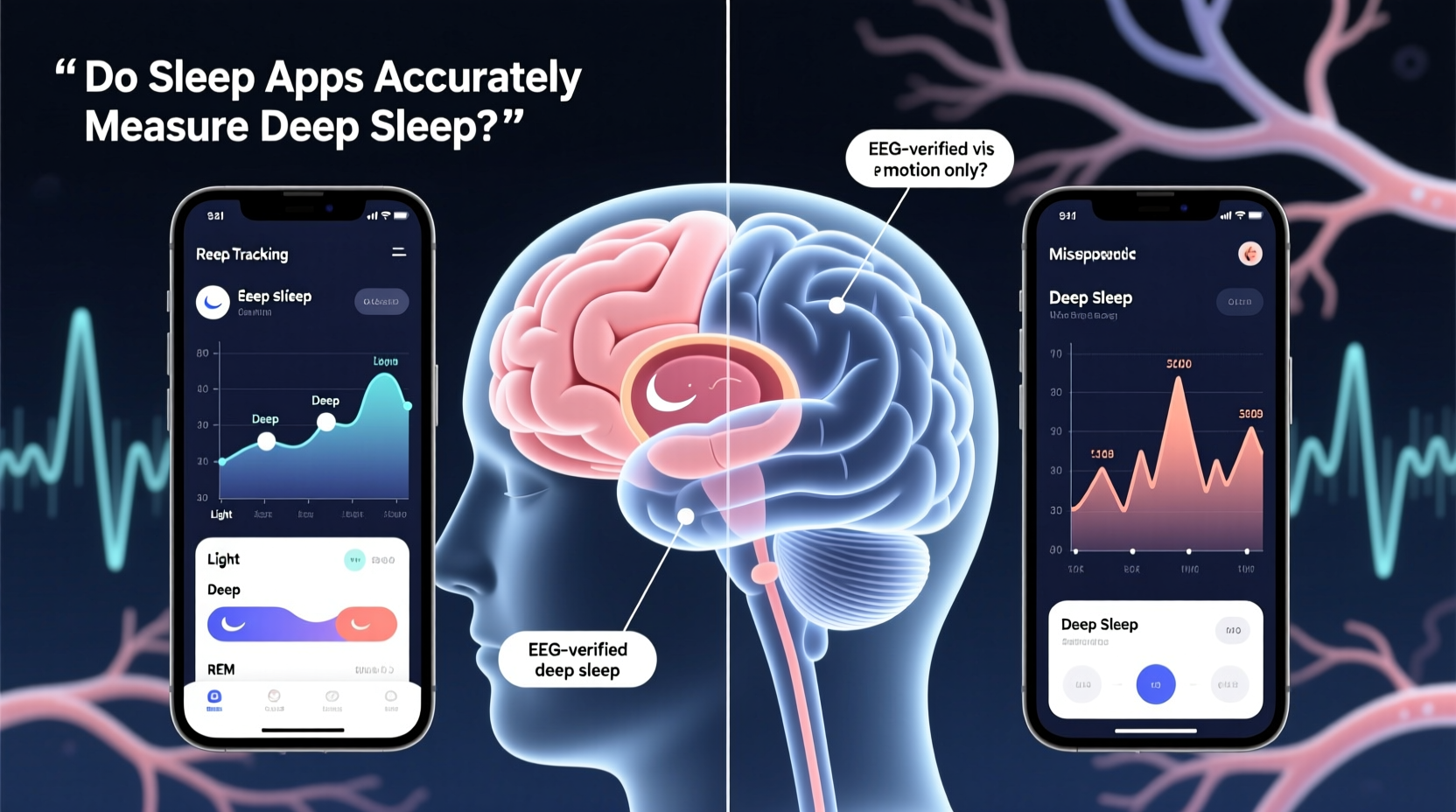
Sleep is a cornerstone of health, influencing everything from cognitive performance to immune function. Among the most critical phases of rest is deep sleep—the stage where the body repairs tissues, consolidates memories, and restores energy. As interest in optimizing sleep grows, so does reliance on sleep tracking apps and wearable devices that claim to monitor these stages. But how accurate are they when it comes to measuring deep sleep?
While modern technology has made sleep data more accessible than ever, the precision behind these metrics varies widely. Understanding the capabilities and limitations of consumer-grade sleep trackers is essential for anyone using them to improve their rest or manage health conditions.
How Sleep Stages Are Scientifically Defined
Sleep is not a uniform state but a dynamic cycle composed of distinct stages, each with unique physiological characteristics. These stages are categorized by the American Academy of Sleep Medicine (AASM) into two main types: non-rapid eye movement (NREM) sleep and rapid eye movement (REM) sleep.
NREM sleep consists of three stages:
- N1 (Light Sleep): The transition phase between wakefulness and sleep, lasting just a few minutes.
- N2 (Intermediate Sleep): A deeper but still relatively light stage, marked by decreased heart rate and lowered body temperature.
- N3 (Deep Sleep): Also known as slow-wave sleep (SWS), this is the most restorative phase, characterized by synchronized brain waves (delta waves), minimal muscle activity, and high arousal thresholds.
Following NREM cycles, REM sleep occurs, associated with vivid dreaming, rapid eye movements, and temporary muscle paralysis. A full sleep cycle lasts about 90 minutes and repeats four to six times per night, with deep sleep dominating the first half of the night.
In clinical settings, polysomnography (PSG) remains the gold standard for sleep staging. It uses multiple sensors to record brain activity (EEG), eye movements (EOG), muscle tone (EMG), heart rhythm (ECG), and breathing patterns. This comprehensive data allows trained technicians to classify sleep stages with high accuracy—especially deep sleep.
How Consumer Sleep Trackers Estimate Deep Sleep
Unlike medical-grade equipment, consumer sleep trackers do not use EEG to directly measure brain waves. Instead, they rely on indirect proxies such as movement, heart rate variability (HRV), and respiratory patterns collected through accelerometers and optical heart rate sensors—commonly found in smartwatches and fitness bands.
Most algorithms follow this general process:
- Movement Detection: Devices use actigraphy—measuring motion via an accelerometer—to infer whether you’re asleep or awake. Prolonged inactivity suggests sleep onset.
- Heart Rate and HRV Analysis: During deep sleep, heart rate drops and becomes more regular, while HRV increases due to parasympathetic dominance. Trackers use these trends to estimate sleep stages.
- Pattern Recognition: Machine learning models trained on limited PSG-correlated datasets attempt to match physiological patterns to likely sleep stages.
Some newer devices, like certain models from Oura Ring or Fitbit, incorporate additional sensors (e.g., skin temperature, blood oxygen levels) to refine estimates. However, none currently offer direct neural monitoring outside clinical environments.
Accuracy Compared to Polysomnography: What Research Shows
The central question remains: can wrist-worn trackers reliably identify deep sleep? Multiple studies have evaluated this, often comparing consumer devices against PSG results in controlled settings.
A 2020 meta-analysis published in the Journal of Clinical Sleep Medicine reviewed 37 studies assessing the validity of wearable sleep trackers. Key findings included:
- Devices were reasonably accurate at detecting total sleep time and wake periods.
- They performed moderately well in identifying light and REM sleep.
- Deep sleep detection showed the highest variability, with overestimation being common.
For example, one study found that Fitbit Charge 2 overestimated deep sleep by up to 45 minutes per night compared to PSG. Another trial involving Garmin wearables showed moderate correlation (r = 0.65) for deep sleep duration but poor agreement in timing and fragmentation.
Dr. Cathy Goldstein, a neurologist and sleep specialist at the University of Michigan, explains:
“Actigraphy-based devices are useful for tracking trends over time, but they shouldn’t be used to diagnose sleep disorders. They lack the resolution to distinguish subtle EEG changes that define true deep sleep.” — Dr. Cathy Goldstein, MD, MS
The fundamental limitation lies in inference. Without EEG, trackers cannot detect delta wave activity—the definitive biomarker of N3 sleep. Instead, they assume deep sleep based on low movement and stable heart rate, which may also occur during quiet N2 sleep or even wakefulness in relaxed individuals.
Factors That Influence Tracking Accuracy
Even within the constraints of indirect measurement, several variables affect how closely a tracker approximates reality:
| Factor | Impact on Accuracy | Why It Matters |
|---|---|---|
| User Physiology | High | Variations in heart rate, skin conductivity, and metabolism affect sensor readings. |
| Device Placement | Medium | Loose fit or incorrect positioning reduces signal quality, especially for optical HR sensors. |
| Sleep Environment | Low-Medium | Noise, light, or partner movement may influence perceived restlessness. |
| Algorithm Version | High | Software updates can significantly change how stages are classified—even retroactively. |
| Individual Sleep Patterns | High | People with insomnia, sleep apnea, or frequent awakenings challenge algorithm assumptions. |
Additionally, proprietary algorithms are rarely transparent. Companies like Apple, Fitbit, and Whoop do not disclose the exact methods used to classify sleep stages, making independent validation difficult.
Mini Case Study: John’s Experience with Inconsistent Readings
John, a 38-year-old software engineer, began using a popular smartwatch to monitor his sleep after experiencing daytime fatigue. Over two weeks, the app reported he was getting 90–110 minutes of deep sleep nightly—well above average for his age group. Surprised, he decided to undergo a home sleep test using a medically approved portable EEG device.
The results revealed a stark discrepancy: John averaged only 45 minutes of actual deep sleep. His tracker had misclassified long stretches of stable N2 sleep as deep sleep due to low movement and consistent heart rate. Upon reviewing his lifestyle, John realized he often lay still with his eyes closed while stressed, creating false signals of deep rest.
This case highlights a critical issue: high numbers don’t always mean better quality. Misleading data can create a false sense of security, delaying necessary interventions for underlying sleep issues.
When Sleep Trackers Are Most Useful (and When They’re Not)
Despite their limitations, sleep tracking apps provide value in specific contexts:
- Trend Monitoring: While absolute values may be off, consistent nightly tracking can reveal patterns—such as reduced deep sleep during stressful weeks or improvements after adjusting bedtime routines.
- Behavioral Feedback: Seeing data can motivate healthier habits like maintaining a regular sleep schedule or reducing evening screen time.
- Screening Tool: Persistent reports of low deep sleep or fragmented rest may prompt users to seek professional evaluation.
However, they fall short when:
- Used for diagnosing sleep disorders like narcolepsy or sleep apnea.
- Interpreted as medically precise without clinical correlation.
- Relying solely on deep sleep duration as a health metric, ignoring overall sleep architecture and subjective restfulness.
Checklist: Getting the Most Out of Your Sleep Tracker
To maximize reliability and usefulness, follow these steps:
- Wear the device consistently every night, ideally on the same wrist.
- Ensure a snug fit—about one finger width from the wrist bone—for optimal heart rate sensing.
- Sync and review data weekly to identify trends, not daily noise.
- Compare objective data with subjective feelings: Do you feel rested when deep sleep is high?
- Pair tracking with journaling—note caffeine, stress, exercise, and bedtime—to contextualize results.
- Update firmware regularly to benefit from algorithm improvements.
- Consult a sleep specialist if patterns suggest chronic disruption or insufficient rest.
Frequently Asked Questions
Can smartphone apps accurately detect deep sleep without wearing a device?
Most phone-based apps use microphone and accelerometer data to detect sounds and movements during sleep. These are significantly less accurate than wearables and cannot estimate heart rate or HRV. While they may detect sleep-wake cycles crudely, they lack the capability to meaningfully assess deep sleep stages.
Are medical sleep studies still necessary if I use a tracker?
Yes. If you experience symptoms like excessive daytime sleepiness, loud snoring, gasping at night, or unrefreshing sleep despite adequate duration, a clinical evaluation is essential. Consumer devices cannot replace diagnostic testing for conditions like obstructive sleep apnea or periodic limb movement disorder.
Which wearable has the best deep sleep tracking accuracy?
Studies suggest that devices incorporating multi-modal sensing—like the Oura Ring (temperature, HRV, movement) and certain Fitbit models with enhanced algorithms—tend to perform better than basic fitness bands. However, no consumer device matches PSG accuracy. Independent research from institutions like Stanford and UC San Francisco continues to evaluate emerging technologies.
Conclusion: Using Data Wisely for Better Sleep
Sleep tracking apps offer a window into your rest—but it’s a distorted one. While they can approximate deep sleep using heart rate and movement, they lack the neurological precision required for definitive staging. Overreliance on these numbers risks misinterpretation, especially when taken out of context.
Their greatest strength lies not in pinpoint accuracy but in longitudinal insight. When used mindfully, these tools can help identify lifestyle influences on sleep quality and encourage healthier behaviors. But they should complement—not replace—clinical expertise and self-awareness.
If you're tracking sleep to optimize health, start by asking not just \"how much deep sleep did I get?\" but \"how do I feel in the morning?\" Combine data with introspection, and when in doubt, consult a sleep professional. True restorative sleep isn't just what the graph shows—it's how your body and mind respond to it.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?