Erectile dysfunction (ED) affects millions of men worldwide, often impacting self-esteem, relationships, and overall quality of life. While occasional difficulty achieving or maintaining an erection is normal, persistent issues may signal an underlying health condition. Accurate diagnosis is essential—not only to restore sexual function but also to uncover potential cardiovascular, hormonal, or psychological concerns. Modern medicine offers a range of reliable diagnostic tools and structured evaluation protocols that allow healthcare providers to pinpoint the root cause and tailor effective treatment plans.
Comprehensive Clinical Evaluation
The diagnostic process for ED begins with a thorough clinical assessment. This includes a detailed patient history, physical examination, and open discussion about sexual health. Physicians aim to understand the onset, duration, and severity of symptoms, as well as any contributing lifestyle factors such as smoking, alcohol use, stress, or lack of physical activity.
During the consultation, doctors typically ask specific questions about:
- Frequency and consistency of erections
- Morning or nocturnal erections (a key indicator of organic vs. psychological causes)
- Presence of libido or sexual desire
- History of chronic conditions like diabetes, hypertension, or heart disease
- Medication use, including prescription drugs, supplements, or recreational substances
- Past pelvic trauma or surgeries
“More than half of ED cases have a vascular origin. A careful history can differentiate between psychogenic and organic etiologies before any lab work is ordered.” — Dr. Alan Rosen, Urologist and Sexual Health Specialist
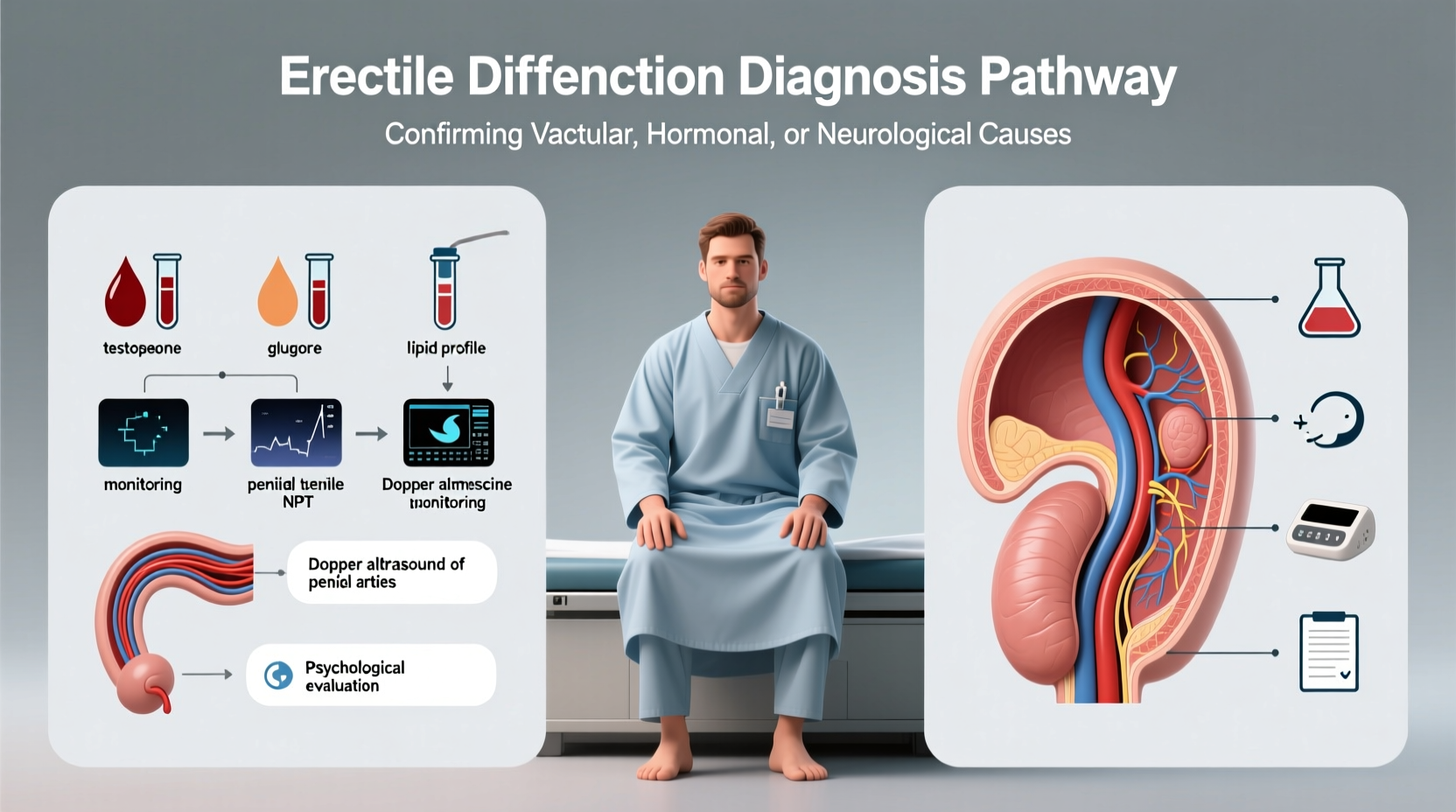
Laboratory Testing for Underlying Conditions
Blood tests are a cornerstone of ED diagnosis because they help identify systemic conditions that impair erectile function. These tests are non-invasive and typically conducted after fasting.
Key laboratory assessments include:
| Test | Purpose | Normal Range / Notes |
|---|---|---|
| Total Testosterone | Evaluates for hypogonadism | 300–1000 ng/dL; low levels may reduce libido and erectile capacity |
| Fasting Glucose & HbA1c | Assesses for diabetes | HbA1c <5.7% normal; elevated levels damage blood vessels and nerves |
| Lipid Panel | Detects dyslipidemia | High cholesterol contributes to atherosclerosis, reducing penile blood flow |
| Prolactin | Rules out pituitary tumors | Elevated levels suppress testosterone production |
| Thyroid Function (TSH) | Identifies hypo/hyperthyroidism | Thyroid imbalances affect energy, mood, and sexual function |
In addition to hormone and metabolic screening, inflammatory markers and liver/kidney function may be evaluated if other comorbidities are suspected.
Specialized Diagnostic Tools and Procedures
When initial evaluations are inconclusive, physicians may recommend advanced diagnostic tests to assess the physiological mechanisms behind ED.
Nocturnal Penile Tumescence (NPT) Testing
NPT measures erections during sleep using a portable device worn overnight. Healthy men typically experience 3–5 full erections per night during REM sleep. Absence of nocturnal erections suggests a physical cause—such as vascular or neurological impairment—while preserved NPT points toward psychological factors.
Penile Doppler Ultrasound
This imaging test evaluates blood flow in the penis. After injecting a vasoactive agent (like alprostadil) to induce an erection, ultrasound waves measure arterial inflow and venous leakage. Key metrics include:
- Systolic peak velocity (SPV): >25 cm/sec indicates healthy arterial supply
- End-diastolic velocity (EDV): <5 cm/sec suggests minimal venous leak
Abnormal results help determine whether revascularization surgery or other interventions might be appropriate.
Dynamic Infusion Cavernosometry (DIC)
A more invasive test used in complex cases, DIC involves injecting fluid into the corpora cavernosa to measure pressure and detect venous leakage. It’s typically reserved for younger men with traumatic ED considering surgical correction.
Psychological and Lifestyle Assessment
Not all ED stems from physical causes. Psychological factors—including depression, anxiety, performance pressure, and relationship conflicts—account for up to 20% of cases, often overlapping with organic conditions.
Clinicians may use validated questionnaires such as:
- International Index of Erectile Function (IIEF)
- Sexual Health Inventory for Men (SHIM)
- Beck Depression Inventory (BDI)
These tools quantify symptom severity and track progress over time. Referral to a psychologist or sex therapist is common when emotional or relational issues dominate the clinical picture.
“Many men feel isolated by ED, but it's one of the most treatable sexual health conditions—especially when diagnosed correctly.” — Dr. Lena Patel, Clinical Psychologist and Sexual Wellness Advisor
Mini Case Study: John’s Journey to Diagnosis
John, a 52-year-old accountant, noticed increasing difficulty maintaining erections over six months. Initially embarrassed, he avoided discussing it with his doctor. After encouragement from his partner, he sought care. His physician reviewed his history—he had type 2 diabetes and took beta-blockers for hypertension—and ordered blood work. Results showed low testosterone (240 ng/dL) and elevated HbA1c (8.1%). A penile Doppler ultrasound revealed reduced arterial inflow (SPV: 18 cm/sec).
With this data, John was diagnosed with mixed organic ED due to vascular disease and hypogonadism. He began testosterone replacement therapy, optimized his diabetes management, and started taking a PDE5 inhibitor. Within three months, erectile function improved significantly. His case highlights how combining clinical insight with targeted testing leads to precise, effective treatment.
Step-by-Step Guide to Getting Diagnosed
If you're experiencing persistent ED, follow this practical timeline to ensure a thorough evaluation:
- Track Symptoms (1–2 weeks): Note frequency, rigidity, associated pain, and presence of morning erections.
- Schedule a Primary Care Visit: Discuss symptoms openly and request basic bloodwork (testosterone, glucose, lipids).
- Review Medications: Ask your doctor if any current prescriptions could contribute to ED.
- See a Specialist (if needed): A urologist can perform advanced tests like Doppler ultrasound or NPT.
- Address Psychological Factors: Consider counseling if stress, anxiety, or relationship issues are present.
- Begin Treatment Plan: Whether lifestyle changes, medication, or therapy, start under medical supervision.
- Follow Up in 6–8 Weeks: Reassess response and adjust approach as necessary.
Common Mistakes to Avoid During Diagnosis
Men seeking answers about ED often encounter misconceptions or delays. Avoid these pitfalls:
- Self-diagnosing with internet searches – Symptoms overlap across conditions; professional input is crucial.
- Skipping lab tests – Assuming ED is “just stress” may miss serious conditions like undiagnosed diabetes.
- Using unregulated supplements – Many over-the-counter “male enhancement” products lack evidence and may interact with medications.
- Delaying care due to embarrassment – Early diagnosis improves outcomes and may reveal life-threatening conditions.
FAQ
Can ED be diagnosed without blood tests?
While a preliminary assessment can be made based on history and symptoms, blood tests are essential to rule out hormonal imbalances, diabetes, and cardiovascular risks. They are standard in modern ED evaluation.
Is psychological ED real? How is it diagnosed?
Yes, psychological ED is real and common, especially in younger men. It’s often diagnosed when physical exams and lab results are normal, but the patient reports sudden onset linked to stress, anxiety, or relationship problems. Preserved nocturnal erections support this diagnosis.
How long does the diagnostic process take?
Initial evaluation usually takes one to two visits over 1–2 weeks. Specialized tests like Doppler ultrasound may require additional appointments, but most diagnoses are established within a month.
Conclusion
Accurately diagnosing erectile dysfunction requires a multifaceted approach—blending patient history, laboratory analysis, imaging, and psychological insight. No single test provides all the answers, but together, these methods form a comprehensive picture that guides effective treatment. Ignoring ED can mean missing early signs of heart disease, diabetes, or hormonal disorders. By seeking timely, evidence-based care, men can not only regain sexual confidence but also improve their long-term health and well-being.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?