Spider veins—those thin, web-like clusters of red, blue, or purple veins visible just beneath the skin—are a common cosmetic concern affecting millions. While typically harmless, they can cause discomfort and impact self-confidence, especially when appearing on the legs or face. The good news is that modern medicine and lifestyle adjustments offer safe, effective solutions. From minimally invasive clinical procedures to daily habits that improve circulation, eliminating spider veins doesn’t require guesswork. This guide outlines evidence-based methods to treat and prevent spider veins, emphasizing safety, sustainability, and real results.
Understanding Spider Veins: Causes and Risk Factors
Spider veins, medically known as telangiectasias, occur when small blood vessels dilate and become visible under the skin. Unlike varicose veins, which are larger and often bulge, spider veins are flat and closer to the surface. They commonly appear on the thighs, calves, ankles, and sometimes the face.
The primary cause is weakened or damaged valves in the veins, leading to poor blood flow and pooling. Several factors increase the likelihood of developing spider veins:
- Genetics: A family history of vein issues significantly raises risk.
- Prolonged standing or sitting: Occupations requiring long periods on your feet (e.g., nursing, teaching) contribute to venous pressure.
- Hormonal changes: Pregnancy, menopause, and birth control use affect vein wall elasticity.
- Age: Vein valves weaken over time, increasing susceptibility after age 50.
- Obesity: Excess weight puts additional pressure on leg veins.
- Sun exposure: On the face, UV damage can trigger facial spider veins.
Clinical Treatments That Work
For visible or bothersome spider veins, several medical treatments offer high success rates with minimal downtime. These should be administered by qualified healthcare providers such as dermatologists or vascular specialists.
Sclerotherapy
This is the most widely used and effective treatment for leg spider veins. A solution (usually polidocanol or saline) is injected directly into the affected vein, causing it to collapse and gradually fade over several weeks. Most patients see improvement within 3–6 weeks, with optimal results after 1–3 sessions.
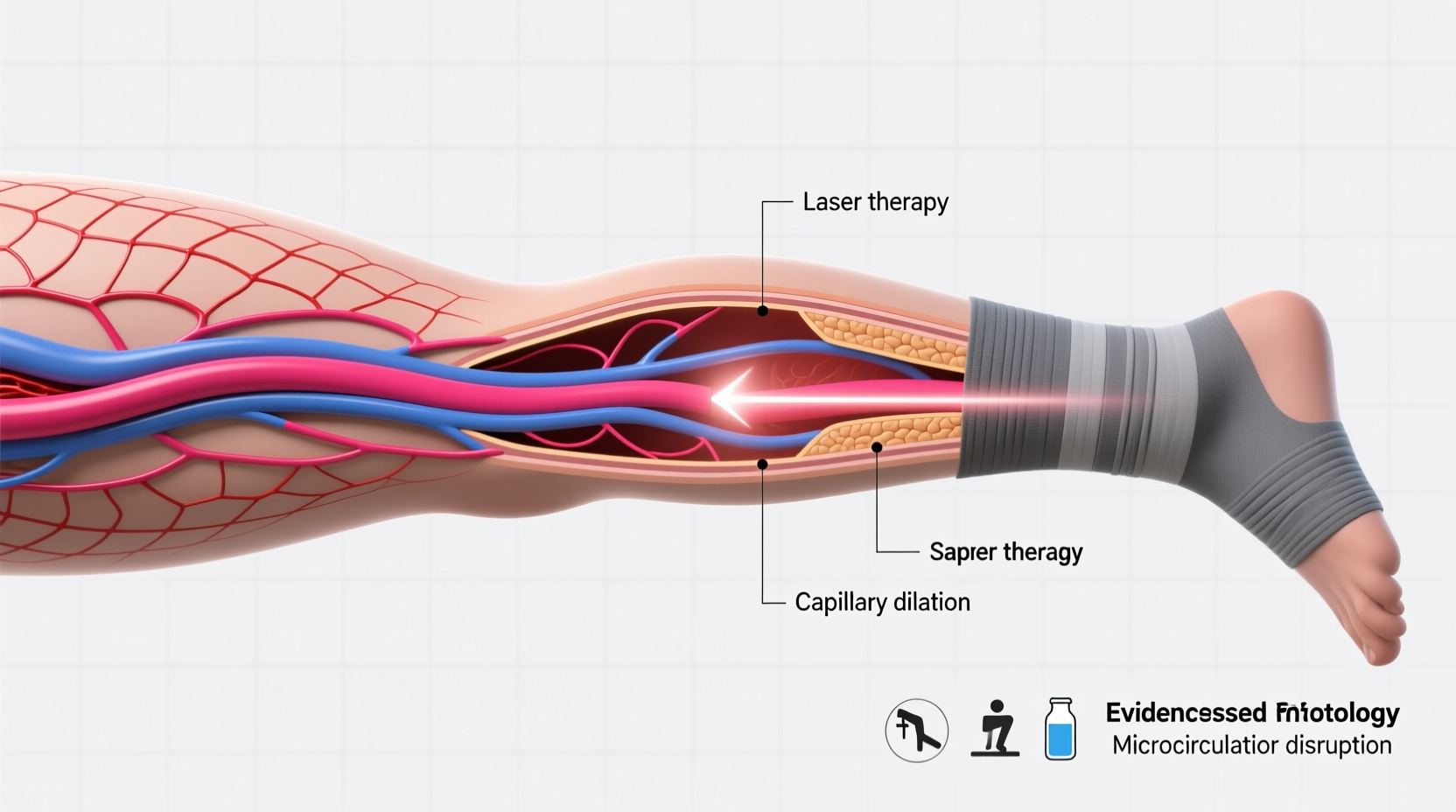
Laser Therapy
Laser treatment uses concentrated light energy to target and destroy small spider veins, particularly those on the face or too fine for injections. It’s non-invasive and ideal for patients wary of needles. Multiple sessions may be needed, but recovery is quick with little to no scarring.
Intense Pulsed Light (IPL)
Similar to laser therapy but using broad-spectrum light, IPL effectively treats facial spider veins caused by sun damage or rosacea. It’s less precise than lasers but covers larger areas efficiently.
“Sclerotherapy remains the gold standard for leg telangiectasias. When performed correctly, it offers over 80% clearance with excellent patient satisfaction.” — Dr. Lena Reyes, Vascular Dermatologist
Step-by-Step Guide to Safe Treatment
If you’re considering professional treatment, follow this timeline to ensure safety and effectiveness:
- Consultation (Week 1): Schedule an evaluation with a board-certified dermatologist or phlebologist. Discuss medical history, symptoms, and aesthetic goals.
- Diagnostics (Optional): An ultrasound may be used to rule out underlying venous insufficiency.
- Treatment Plan (Week 2): Based on vein size and location, your provider will recommend sclerotherapy, laser, or a combination.
- First Session (Week 3): Begin treatment. Avoid sun exposure and blood-thinning medications beforehand.
- Recovery & Monitoring (Weeks 4–8): Wear compression stockings if advised. Avoid strenuous activity for 48 hours post-treatment.
- Follow-Up Sessions (As Needed): Repeat every 4–6 weeks until desired results are achieved.
- Maintenance (Ongoing): Adopt preventive habits to reduce recurrence.
Lifestyle and Home-Based Prevention Strategies
While clinical treatments remove existing spider veins, long-term prevention relies on daily habits that support healthy circulation. These approaches are safe, cost-effective, and beneficial for overall vascular health.
- Exercise regularly: Walking, cycling, and swimming strengthen calf muscles and promote blood flow.
- Elevate your legs: After long periods of standing or sitting, raise your legs above heart level for 15 minutes to reduce pooling.
- Wear compression stockings: Graduated compression hosiery helps veins move blood more efficiently, reducing pressure and swelling.
- Maintain a healthy weight: Reducing excess body mass decreases strain on leg veins.
- Avoid tight clothing: Belts, girdles, or restrictive pants can impede circulation.
- Limit sun exposure: Use SPF 30+ daily to protect facial capillaries from UV damage.
| Method | Best For | Time to See Results | Risk Level |
|---|---|---|---|
| Sclerotherapy | Leg spider veins | 3–6 weeks | Low (minor bruising, rare pigmentation) |
| Laser Therapy | Facial or fine leg veins | 2–8 weeks | Low (temporary redness, swelling) |
| Compression Stockings | Prevention & symptom relief | Ongoing benefit | None |
| Lifestyle Changes | All cases, especially early-stage | Months of consistent practice | None |
Real-World Example: Sarah’s Experience
Sarah, a 42-year-old teacher from Portland, noticed spider veins forming on her calves after years of standing during class. Initially dismissive, she began experiencing mild aching and self-consciousness about wearing skirts. She consulted a vascular specialist who confirmed no deeper venous disease and recommended sclerotherapy.
After three monthly sessions and consistent use of compression stockings, Sarah’s leg veins faded by over 80%. She also incorporated 30-minute walks into her routine and now performs leg elevation exercises nightly. Two years later, only minor touch-ups were needed. “It wasn’t just about looks,” she said. “My legs feel lighter, and I finally wear shorts again without hesitation.”
Frequently Asked Questions
Are spider veins dangerous?
In most cases, spider veins are not dangerous and are primarily a cosmetic concern. However, if accompanied by pain, swelling, or heaviness, they may indicate underlying venous insufficiency, which requires medical evaluation.
Can spider veins come back after treatment?
Treated veins do not return, but new ones can develop over time, especially without preventive measures. Maintaining a healthy lifestyle and wearing compression garments when necessary reduces recurrence.
Is treatment covered by insurance?
Most insurance plans consider spider vein removal cosmetic and do not cover it. However, if symptoms like pain or swelling are present and linked to venous disease, partial coverage may apply. Always check with your provider.
Final Thoughts: Taking Action with Confidence
Getting rid of spider veins safely doesn’t mean choosing between ineffective home remedies and risky procedures. With access to advanced treatments like sclerotherapy and laser therapy—and the power of simple lifestyle upgrades—managing spider veins is both achievable and sustainable. The key is starting with a proper diagnosis, selecting evidence-based methods, and committing to long-term vein health.
Whether you're seeking relief from discomfort or simply want clearer skin, taking informed steps today can lead to lasting confidence tomorrow. Don’t let spider veins hold you back from feeling your best.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?