Hematocrit—the percentage of red blood cells in your total blood volume—is a critical marker of cardiovascular efficiency, oxygen delivery, and overall vitality. When hematocrit is too low, it can lead to fatigue, shortness of breath, and reduced physical performance. While extremely high levels pose risks, modestly increasing hematocrit within the normal range (typically 38–50% for adults) can enhance stamina, cognitive function, and metabolic health. The key lies in doing so safely and sustainably, without resorting to risky shortcuts like blood doping or unregulated supplements.
This guide explores evidence-based methods to support healthy red blood cell production, optimize iron metabolism, and improve oxygen-carrying capacity through nutrition, lifestyle adjustments, and medical awareness—all designed to promote long-term well-being.
Understanding Hematocrit and Why It Matters
Hematocrit reflects how much space red blood cells occupy in your bloodstream. These cells contain hemoglobin, which binds oxygen in the lungs and delivers it to tissues throughout the body. A low hematocrit often signals anemia, dehydration, chronic disease, or nutritional deficiencies. Conversely, chronically elevated levels may indicate polycythemia, smoking-related hypoxia, or kidney disorders.
Optimal hematocrit supports aerobic capacity, mental clarity, and recovery from physical exertion. Athletes, individuals living at high altitudes, and those recovering from illness often benefit from slightly higher hematocrit—provided it remains within safe physiological limits.
“Maintaining balanced hematocrit isn’t about chasing numbers—it’s about ensuring efficient oxygen transport, which underpins nearly every system in the body.” — Dr. Lena Torres, Hematology Specialist, Mayo Clinic
Nutritional Foundations for Red Blood Cell Production
The body requires specific nutrients to manufacture red blood cells effectively. Deficiencies in iron, vitamin B12, folate, and copper are among the most common causes of low hematocrit.
Key Nutrients and Their Food Sources
| Nutrient | Role in Hematocrit | Top Food Sources |
|---|---|---|
| Iron | Essential for hemoglobin synthesis | Grass-fed beef, lentils, spinach, pumpkin seeds, oysters |
| Vitamin B12 | Supports DNA synthesis in red blood cells | Salmon, eggs, dairy, fortified cereals |
| Folate (B9) | Prevents megaloblastic anemia | Dark leafy greens, chickpeas, avocado, broccoli |
| Copper | Aids iron absorption and utilization | Beef liver, cashews, sunflower seeds, lentils |
| Vitamin A | Enhances iron mobilization from storage | Sweet potatoes, carrots, spinach, cod liver oil |
Pairing iron-rich plant foods (non-heme iron) with vitamin C sources—like bell peppers, citrus, or strawberries—can boost absorption by up to 67%. Avoid drinking coffee or tea with meals, as tannins inhibit iron uptake.
Lifestyle Modifications That Support Healthy Hematocrit
Beyond diet, several daily habits influence red blood cell production and oxygen efficiency.
1. Altitude Exposure and Intermittent Hypoxia Training
Living or training at moderate altitudes (5,000–8,000 feet) stimulates erythropoietin (EPO) release from the kidneys, prompting bone marrow to produce more red blood cells. Even short stints—like weekend hikes in mountainous regions—can have cumulative benefits over time.
For those unable to relocate, simulated altitude training using hypoxic tents or masks may offer mild improvements, though results vary and should be approached cautiously under professional guidance.
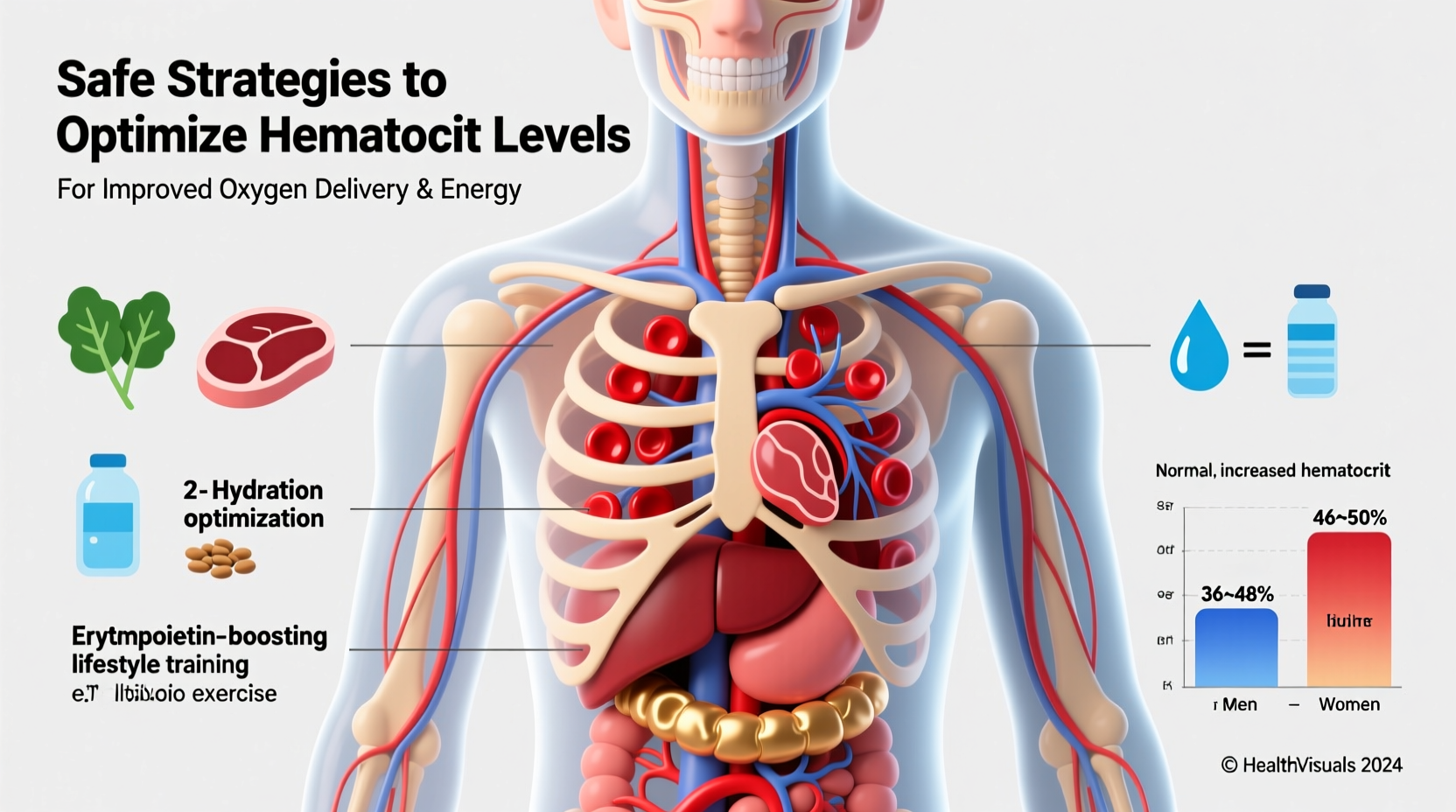
2. Exercise and Cardiovascular Conditioning
Regular aerobic exercise increases plasma volume initially, which may temporarily lower hematocrit. However, sustained training leads to proportional increases in red blood cell mass, improving oxygen delivery efficiency. Endurance athletes often exhibit slightly higher hematocrit due to chronic adaptation.
3. Hydration Management
Dehydration artificially elevates hematocrit by reducing plasma volume, creating a misleadingly high reading. Chronic underhydration masks true red blood cell status. Aim for consistent fluid intake—about 2.7 liters (91 oz) for women and 3.7 liters (125 oz) for men daily, adjusting for climate and activity level.
Medical Considerations and Monitoring
Before attempting to raise hematocrit, confirm your baseline through a complete blood count (CBC). Unexplained low levels warrant investigation into underlying causes such as gastrointestinal bleeding, celiac disease, or chronic inflammation.
If deficiency is confirmed, targeted supplementation may be necessary:
- Iron supplements: Ferrous sulfate, bisglycinate, or fumarate—best taken on an empty stomach with vitamin C, unless gastrointestinal side effects occur.
- Vitamin B12: Sublingual or injectable forms may be needed for those with pernicious anemia or malabsorption.
- Folic acid: Particularly important during pregnancy or in individuals with poor dietary intake.
Always consult a healthcare provider before starting supplements. Excess iron can lead to oxidative stress and organ damage, while unmonitored EPO stimulation poses thrombotic risks.
Mini Case Study: Recovery from Iron-Deficiency Anemia
Maria, a 34-year-old yoga instructor, experienced persistent fatigue and lightheadedness after her second pregnancy. Bloodwork revealed a hematocrit of 33% and ferritin of 12 ng/mL (severely low). Under her doctor’s supervision, she began taking ferrous bisglycinate (100 mg elemental iron daily), increased consumption of lean red meat and lentils, and paired meals with lemon-dressed salads. Within three months, her hematocrit rose to 39%, and energy levels normalized. Follow-up testing ensured she didn’t overshoot optimal ranges.
Step-by-Step Guide to Safely Increase Hematocrit Over 12 Weeks
- Week 1–2: Assess and Test
Get a CBC and iron panel. Review medications and symptoms with a physician. - Week 3–4: Optimize Diet
Incorporate iron-rich foods twice daily. Add vitamin C at each meal. Eliminate inhibitors like tea near meals. - Week 5–6: Begin Targeted Supplementation (if needed)
Start prescribed iron or B12 under medical supervision. Monitor for side effects. - Week 7–8: Introduce Aerobic Training
Add 30 minutes of brisk walking, cycling, or swimming 4–5 times weekly. - Week 9–10: Evaluate Progress
Repeat blood tests. Adjust dosage or diet based on results. - Week 11–12: Stabilize and Maintain
Transition to maintenance doses if applicable. Focus on sustainable habits.
Do’s and Don’ts: Quick Reference Table
| Action | Do | Don’t |
|---|---|---|
| Diet | Eat iron-rich foods with vitamin C | Consume calcium or coffee with iron meals |
| Supplements | Take iron on empty stomach (if tolerated) | Self-prescribe high-dose iron without testing |
| Exercise | Engage in regular cardio | Overtrain, increasing inflammation |
| Hydration | Drink water consistently | Rely on thirst alone as a cue |
| Monitoring | Track bloodwork every 6–12 weeks | Ignore persistently abnormal results |
Frequently Asked Questions
Can I increase hematocrit quickly before a competition?
Attempting rapid elevation—through dehydration, blood transfusions, or EPO abuse—is dangerous and unethical. Natural methods take weeks to show effect. Focus on long-term health rather than short-term manipulation.
Is a higher hematocrit always better?
No. Values above 50% (men) or 46% (women) increase blood viscosity, raising the risk of clots, stroke, and heart strain. Balance is essential.
Does sleep affect hematocrit?
Indirectly, yes. Poor sleep disrupts hormone regulation, including EPO and cortisol, both of which influence red blood cell production. Prioritize 7–9 hours nightly for optimal recovery and metabolic function.
Conclusion: Build Sustainable Blood Health
Improving hematocrit isn’t about chasing extremes—it’s about nurturing the body’s natural ability to carry oxygen efficiently. By focusing on nutrient-dense eating, smart training, and informed medical care, you can support healthy red blood cell levels that enhance energy, resilience, and longevity.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?