Heart disease remains the leading cause of death worldwide, yet many cases are preventable with early detection and consistent monitoring. The key lies in proactive heart health management—knowing when and how to get your heart checked using medically recognized screenings and assessments. This guide walks you through the essential steps, from understanding risk factors to interpreting results, so you can take informed control of your cardiovascular health.
Step 1: Understand Your Personal Risk Factors
Before scheduling any test, assess your baseline risk for heart disease. Some factors are modifiable; others are not. Recognizing them helps determine how urgently and frequently you should pursue screenings.
- Non-modifiable risks: Age (men over 45, women over 55), family history of early heart disease, genetic predispositions.
- Modifiable risks: High blood pressure, high cholesterol, smoking, obesity, physical inactivity, diabetes, poor diet, chronic stress.
If two or more risk factors apply to you—especially if there’s a family history—it’s wise to begin regular cardiac evaluations earlier than standard guidelines suggest.
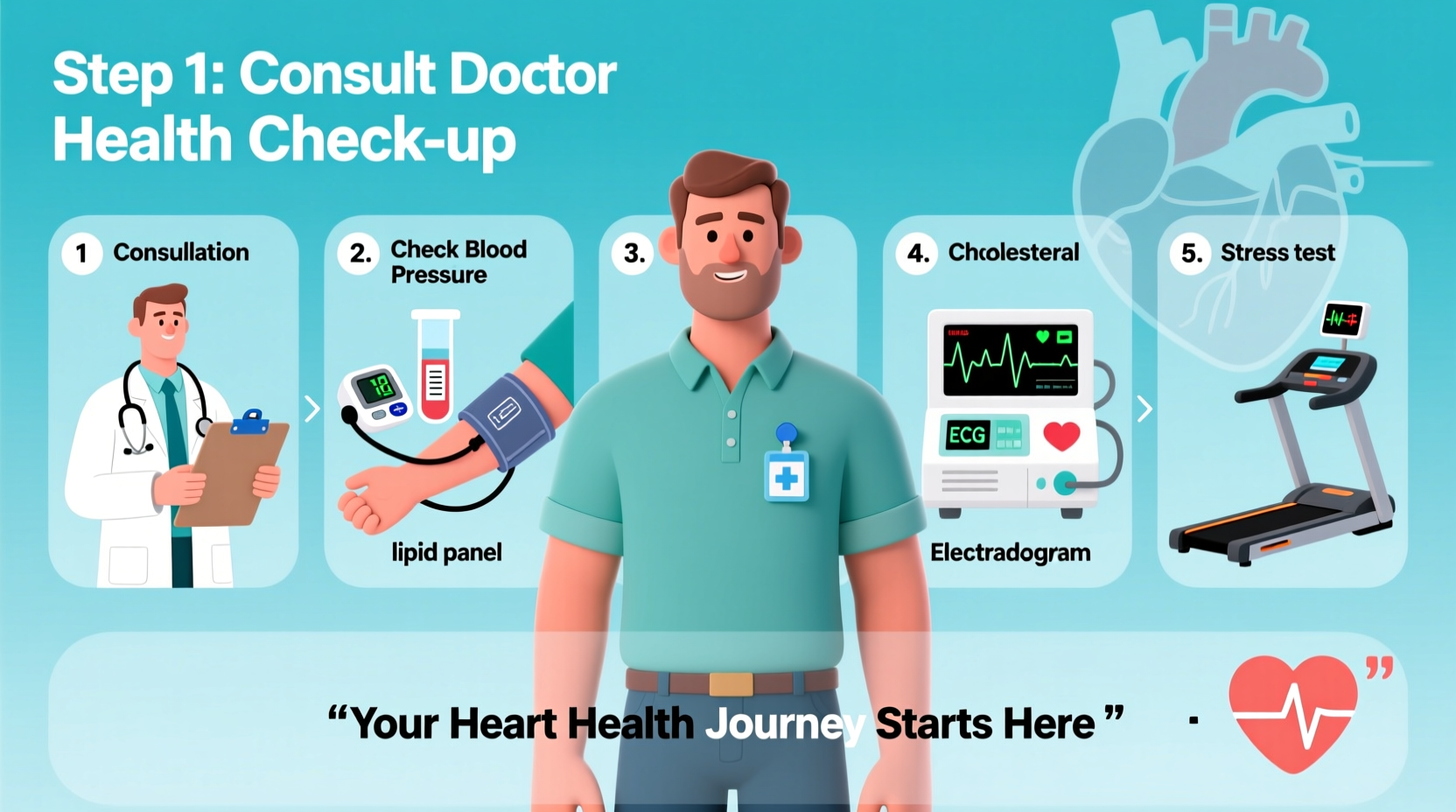
Step 2: Schedule a Preventive Check-Up with Your Primary Care Provider
Your first formal step should be a consultation with your primary care physician. They will review your medical history, lifestyle habits, and initial vitals. This visit typically includes:
- Blood pressure measurement
- Body mass index (BMI) and waist circumference assessment
- Preliminary blood work (fasting lipid panel, glucose levels)
- Discussion of symptoms like fatigue, dizziness, or chest tightness
Based on this evaluation, your doctor may recommend further testing or refer you to a cardiologist for specialized assessment.
“Early intervention is the most powerful tool we have against heart disease. Many patients don’t realize they’re at risk until it’s too late.” — Dr. Lena Patel, Preventive Cardiologist, Cleveland Clinic
Step 3: Complete Essential Heart Screenings
The following tests form the foundation of a comprehensive heart check. Not all are needed annually, but their frequency depends on age, risk level, and prior results.
| Test | What It Measures | Recommended Frequency | Preparation Needed |
|---|---|---|---|
| Blood Pressure Check | Force of blood against artery walls | At least once every 2 years (annually if elevated) | Rest 5 minutes before test; avoid caffeine beforehand |
| Cholesterol Panel (Lipid Profile) | LDL, HDL, triglycerides, total cholesterol | Every 4–6 years (more often with risk factors) | Fasting for 9–12 hours required |
| Electrocardiogram (ECG/EKG) | Electrical activity of the heart | As needed based on symptoms or risk | None; wear loose clothing |
| Echocardiogram | Heart structure and function via ultrasound | Only if abnormalities detected or symptoms present | None |
| Stress Test | Heart performance under physical exertion | When ECG or symptoms suggest concern | Fasting, avoid caffeine, consult on medication adjustments |
Advanced Assessments (If Indicated)
In higher-risk individuals, additional tools may be used:
- Coronary Calcium Scan: A CT scan that detects calcium buildup in coronary arteries. Highly predictive of future heart events, especially in asymptomatic adults aged 40–75.
- Carotid Intima-Media Thickness (CIMT): Ultrasound measuring arterial wall thickness, indicating early atherosclerosis.
- Cardiac MRI or CT Angiography: Detailed imaging for suspected structural or blockage issues.
Step 4: Interpret Results with Clinical Context
Understanding your numbers is crucial. Here’s what common markers mean:
- Blood Pressure: Ideal is below 120/80 mm Hg. 130/80 or higher indicates hypertension.
- LDL Cholesterol: Less than 100 mg/dL is optimal; above 160 mg/dL is high risk.
- HDL Cholesterol: Above 60 mg/dL is protective; below 40 mg/dL increases risk.
- Triglycerides: Below 150 mg/dL is normal; over 200 mg/dL raises concern.
- A1C: Below 5.7% is normal; 5.7–6.4% indicates prediabetes; 6.5% or higher suggests diabetes.
Results don’t exist in isolation. A slightly elevated LDL might not be alarming in a low-risk person but could prompt immediate action in someone with a strong family history.
Step 5: Create a Heart Health Action Plan
Testing is only useful if followed by action. Work with your doctor to build a personalized strategy based on your results.
Checklist: Building Your Heart Health Plan
- ✅ Set specific goals (e.g., lower LDL by 20 points, reduce systolic BP to under 130)
- ✅ Adopt a heart-healthy diet (Mediterranean-style: rich in vegetables, whole grains, fish, nuts)
- ✅ Aim for 150 minutes of moderate aerobic exercise weekly
- ✅ Quit smoking and limit alcohol to one drink per day (women), two (men)
- ✅ Manage stress through mindfulness, sleep hygiene, or therapy
- ✅ Take prescribed medications consistently (e.g., statins, antihypertensives)
- ✅ Schedule follow-up tests as recommended (usually 3–12 months after intervention)
Real Example: John’s Preventive Turnaround
John, a 52-year-old accountant, had no symptoms but a father who suffered a heart attack at 58. During a routine check-up, his LDL was 178 mg/dL and blood pressure 142/90 mm Hg. His doctor ordered a coronary calcium scan, which revealed a score of 210—indicating significant plaque buildup.
Instead of waiting for an event, John began a regimen: daily walking, dietary changes, and a low-dose statin. Within nine months, his LDL dropped to 98 mg/dL, and his blood pressure normalized. Repeat screening showed stabilized calcification. Early detection gave him a second chance.
Frequently Asked Questions
At what age should I start getting my heart checked?
Baseline screenings like blood pressure and cholesterol should begin at age 20. More targeted assessments start around age 35–40, or earlier if you have risk factors such as obesity, diabetes, or family history.
Can I get heart screenings without a referral?
Some labs offer direct-to-consumer blood panels, and some imaging centers provide self-referred calcium scans. However, interpreting results without clinical context can be misleading. It’s best to involve a healthcare provider to ensure appropriate testing and follow-up.
Are heart screenings covered by insurance?
Most preventive screenings—blood pressure checks, cholesterol panels, and certain ECGs—are fully covered under the Affordable Care Act when performed during annual wellness visits. Advanced tests like calcium scans may require out-of-pocket payment unless medically indicated.
Conclusion: Take Charge Before Symptoms Appear
Your heart works tirelessly, often without complaint—until it can’t. The power of modern cardiology lies not in treating heart attacks, but in preventing them. By following a structured approach to heart health—assessing risk, scheduling key screenings, understanding results, and acting decisively—you gain the upper hand over silent threats like hypertension and atherosclerosis.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?