Occasional muscle twitches are a normal part of human physiology. When your left bicep suddenly flutters or jumps beneath the skin, it can be surprising—but in most cases, not dangerous. These involuntary contractions, known as fasciculations, affect people of all ages and fitness levels. While often harmless, persistent or worsening twitching may signal underlying issues that require medical evaluation. Understanding the difference between benign twitches and those warranting concern empowers you to make informed decisions about your health.
What Causes Left Bicep Twitching?
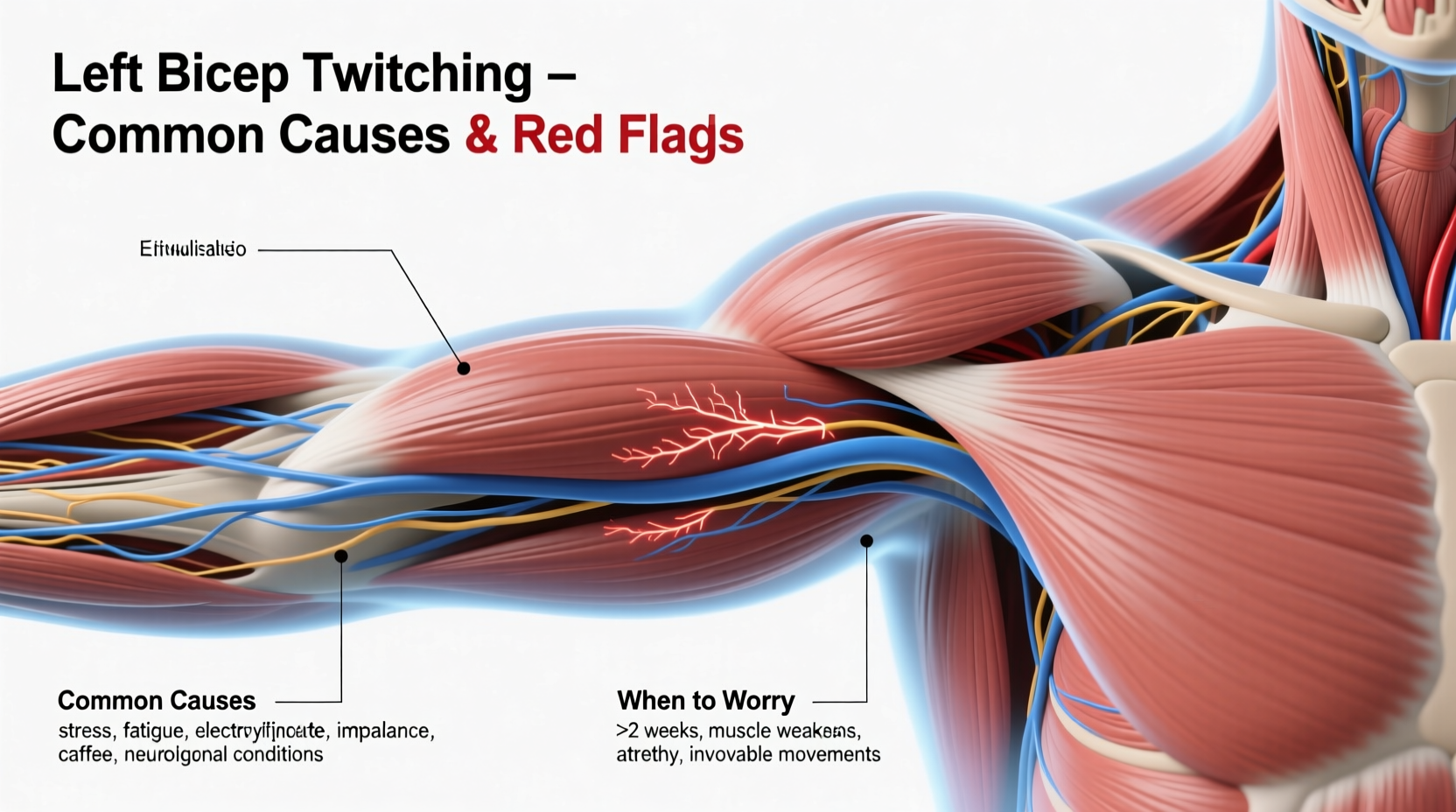
Muscle fasciculations in the bicep occur when small groups of muscle fibers contract spontaneously due to nerve signaling irregularities. The left bicep is no more prone than the right, but because many people are right-handed, minor imbalances in muscle use or stress patterns may influence perception. Common triggers include:
- Stress and anxiety: Elevated cortisol and adrenaline levels increase neuromuscular excitability.
- Physical exertion: Overuse from weightlifting or repetitive motion can irritate motor neurons.
- Caffeine intake: Stimulants heighten nervous system activity, potentially triggering twitches.
- Sleep deprivation: Poor recovery disrupts electrolyte balance and neural regulation.
- Dehydration or electrolyte imbalance: Low magnesium, potassium, or calcium impair nerve-muscle communication.
- Nerve compression: Issues in the cervical spine (neck) may affect nerves leading to the arm.
When Is Left Bicep Twitching Normal?
Benign fasciculation syndrome (BFS) accounts for the majority of isolated muscle twitches. It’s characterized by intermittent, painless muscle flickers without weakness or atrophy. If your left bicep twitching meets the following criteria, it’s likely not a cause for immediate concern:
- Lasts seconds to minutes and resolves on its own
- Occurs sporadically, not daily or continuously
- Doesn’t spread to other muscles
- No associated muscle weakness, cramping, or loss of coordination
- Improves with rest, hydration, or reduced stress
Many athletes notice bicep twitching after intense training sessions—this is typically due to localized fatigue and microtrauma to muscle fibers. As long as strength remains intact and movement is unaffected, such twitches are part of normal recovery.
Red Flags: When to Seek Medical Attention
While most cases resolve independently, certain symptoms suggest the need for clinical evaluation. Persistent or progressive twitching could indicate neurological conditions such as peripheral neuropathy, radiculopathy, or, rarely, motor neuron diseases like ALS (amyotrophic lateral sclerosis).
“Not every muscle twitch signals disease, but persistent fasciculations combined with weakness or atrophy should prompt neurologic assessment.” — Dr. Lena Patel, Neurologist, Cleveland Clinic
Seek prompt medical advice if you experience any of the following:
- Twitching that lasts for weeks without improvement
- Spreading to adjacent muscles (forearm, shoulder, chest)
- Noticeable muscle weakness or shrinking (atrophy)
- Frequent cramps or spasms alongside twitching
- Numbness, tingling, or shooting pain down the arm
- Difficulty gripping objects or lifting the arm
Differential Diagnosis Table
| Condition | Symptoms | Typical Duration | Action Required |
|---|---|---|---|
| Benign Fasciculation Syndrome | Intermittent twitches, no weakness | Episodic, resolves with lifestyle changes | Lifestyle adjustment, monitoring |
| Cervical Radiculopathy | Pain, numbness, weakness radiating from neck | Persistent unless treated | Medical imaging, physical therapy |
| Peripheral Neuropathy | Burning, tingling, balance issues | Chronic, progressive | Diabetes screening, neurology consult |
| Motor Neuron Disease (e.g., ALS) | Weakness, atrophy, speech/swallowing issues | Progressive | Urgent neurologic workup |
Step-by-Step Guide to Managing Bicep Twitching
If you're experiencing occasional left bicep twitching, follow this practical timeline to assess and address potential causes:
- Day 1–3: Track Symptoms
Keep a log noting frequency, duration, triggers (e.g., post-workout, high-stress day), and associated sensations. - Day 4–7: Optimize Lifestyle Factors
Reduce caffeine, ensure adequate hydration, consume potassium/magnesium-rich foods (bananas, spinach, nuts), and aim for consistent sleep. - Week 2: Evaluate Progress
If twitching diminishes, continue healthy habits. If unchanged, consider eliminating alcohol and managing stress through mindfulness or yoga. - Week 3–4: Assess for Red Flags
If twitching persists beyond a month or worsens, consult a primary care physician. Mention any family history of neurological disorders. - Month 2+: Medical Workup (if needed)
Possible tests include EMG (electromyography), blood panels (electrolytes, thyroid, vitamin D/B12), and cervical spine imaging.
Real-Life Example: Recognizing Early Warning Signs
Mark, a 42-year-old software developer, noticed his left bicep twitching after a particularly stressful project deadline. Initially dismissing it as fatigue, he observed that over six weeks, the twitching became constant and began spreading to his forearm. He also found himself dropping coffee mugs more frequently and struggling to open jars. Concerned, he visited a neurologist who ordered an EMG test. Results revealed mild ulnar nerve entrapment at the elbow, exacerbated by poor ergonomics and chronic tension. With ergonomic adjustments, physical therapy, and stress management techniques, Mark’s symptoms resolved within two months.
This case illustrates how seemingly minor symptoms can escalate when compounded by lifestyle factors—and why early intervention matters.
Prevention Checklist
To minimize the risk of recurrent bicep twitching, adopt these evidence-based practices:
- ✅ Stay hydrated throughout the day (aim for 2–3 liters of water)
- ✅ Limit caffeine to under 400 mg per day (about 2 cups of coffee)
- ✅ Include magnesium-rich foods: almonds, avocados, dark leafy greens
- ✅ Practice regular stress-reduction techniques: deep breathing, meditation, walking
- ✅ Maintain proper posture, especially during desk work
- ✅ Warm up before exercise and stretch after workouts
- ✅ Get 7–9 hours of uninterrupted sleep nightly
Frequently Asked Questions
Can dehydration cause bicep twitching?
Yes. Dehydration affects electrolyte balance, particularly sodium, potassium, and magnesium, which are essential for normal nerve signaling and muscle contraction. Even mild dehydration can trigger fasciculations, especially after sweating or intense physical activity.
Is left bicep twitching a sign of heart problems?
No, isolated bicep twitching is not a symptom of heart disease. However, chest pain, shortness of breath, or pain radiating down the left arm accompanied by nausea or dizziness should be evaluated immediately as possible signs of cardiac events. Muscle twitching alone does not indicate heart trouble.
How long should I wait before seeing a doctor about muscle twitching?
If the twitching persists beyond four weeks, spreads to other areas, or is accompanied by weakness, atrophy, or pain, schedule a medical consultation. Earlier evaluation is recommended if you have a personal or family history of neurological conditions.
Conclusion: Listen to Your Body, Act with Confidence
Left bicep twitching is usually a fleeting, harmless occurrence tied to lifestyle factors like stress, fatigue, or diet. By addressing root causes—improving sleep, reducing stimulants, staying hydrated—you can often eliminate the issue naturally. But when twitching becomes persistent or is paired with functional changes like weakness or numbness, professional evaluation is essential. Neurological health should never be ignored out of hope or hesitation. Take proactive steps today: monitor your symptoms, adjust your habits, and seek care when needed. Your body communicates for a reason—learn to listen, respond wisely, and maintain long-term well-being.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?