For individuals managing asthma or other chronic respiratory conditions, tracking lung function is not just informative—it’s essential. One of the most accessible and effective tools for daily lung monitoring is the peak flow meter. This small, handheld device measures how quickly you can expel air from your lungs, providing real-time insight into your breathing capacity. When used correctly, peak flow readings help detect early signs of worsening symptoms, guide treatment decisions, and improve long-term respiratory control.
Yet, despite its simplicity, many users fail to achieve consistent, reliable results due to improper technique or inconsistent use. This guide breaks down every element of mastering peak flow measurement—from selecting the right device to interpreting results—with precision and practicality.
Understanding Peak Flow and Why It Matters
Peak expiratory flow (PEF) reflects the maximum speed at which you can forcefully exhale after a full inhalation. It’s measured in liters per minute (L/min) and serves as an indicator of airway openness. In people with asthma, airways can become inflamed and narrowed, reducing airflow and lowering peak flow values—often before symptoms like wheezing or shortness of breath appear.
Regular monitoring allows for early intervention. According to the American Lung Association, “Tracking peak flow regularly helps patients recognize changes in lung function earlier than waiting for symptoms to worsen.” This proactive approach reduces emergency visits and enhances quality of life.
Your personal best peak flow—the highest reading you achieve over a two-week period when your asthma is well-controlled—becomes the benchmark against which future measurements are compared. Changes below 80% of your personal best may signal the onset of an exacerbation.
“Daily peak flow monitoring can be a game-changer for asthma patients. It turns subjective feelings into objective data, empowering both patients and clinicians.” — Dr. Lena Torres, Pulmonologist, Cleveland Clinic
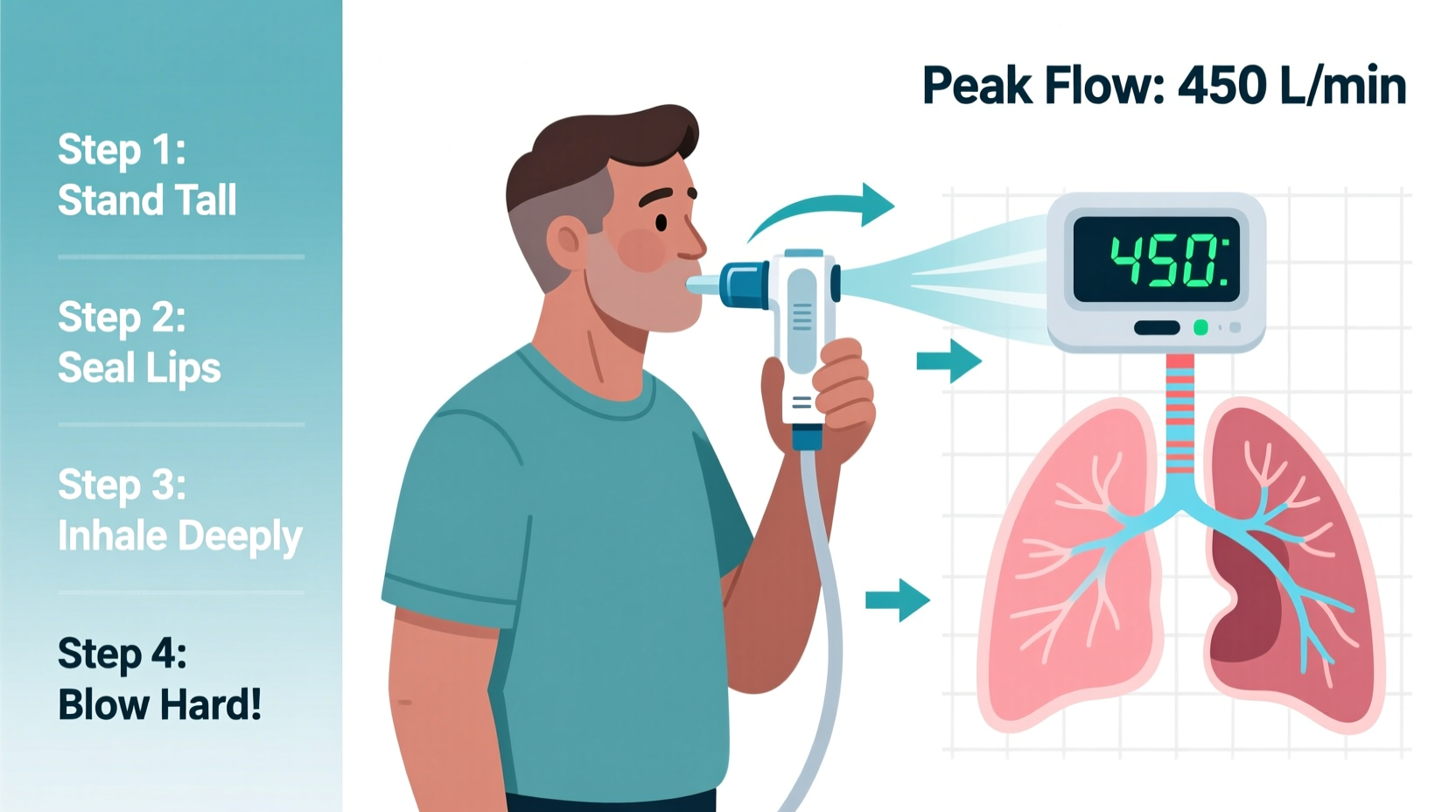
Step-by-Step Guide to Accurate Peak Flow Measurement
To get reliable results, consistency in technique is crucial. Follow this six-step process each time you use your peak flow meter:
- Prepare the Device: Ensure the marker on the scale is reset to zero. Hold the meter horizontally, avoiding tilting that could interfere with the sliding indicator.
- Stand Up Straight: Standing promotes deeper inhalation and more forceful exhalation. If standing isn’t possible, sit upright with good posture.
- Take a Deep Breath: Inhale fully, filling your lungs completely. Do not puff your cheeks or hold your breath before exhaling.
- Seal Your Lips Around the Mouthpiece: Place the mouthpiece between your lips, forming an airtight seal. Avoid placing your tongue inside the tube, as this can block airflow.
- Breathe Out Hard and Fast: Exhale as forcefully and quickly as possible in a single burst. A slow push will not yield an accurate reading.
- Record the Number: Note the value indicated on the scale. Repeat the process two more times, recording all three attempts.
The highest of the three readings is your official peak flow result for that session. Do not average the numbers—use only the top value.
Choosing the Right Peak Flow Meter and Maintaining Accuracy
Not all peak flow meters are created equal. Most fall into one of two categories: mechanical (analog) or digital. Analog meters are affordable and require no batteries but may lose calibration over time. Digital models offer automatic data logging and greater precision but come at a higher cost.
Regardless of type, proper maintenance ensures accuracy:
- Clean the mouthpiece weekly with mild soapy water and allow it to air dry.
- Avoid dropping the device; internal components can shift and affect readings.
- Check calibration annually or if readings seem inconsistent despite good technique.
- Replace the device every 2–3 years or sooner if cracks develop.
| Factor | Do | Avoid |
|---|---|---|
| Position | Stand or sit upright | Slouching or lying down |
| Exhalation | Blast out air fast and hard | Blowing slowly or in stages |
| Lips | Seal tightly around mouthpiece | Letting air leak at corners |
| Frequency | Test twice daily during stable periods | Only checking during flare-ups |
Interpreting Results and Using Zones Effectively
Once you’ve established your personal best, categorize your readings using the traffic light system recommended by the National Asthma Education and Prevention Program (NAEPP):
- Green Zone (80–100% of personal best): Airflow is normal. Continue current medications and routines.
- Yellow Zone (50–79% of personal best): Caution needed. Symptoms may be developing. Follow your asthma action plan—this may include using rescue inhalers or increasing controller meds.
- Red Zone (below 50%): Medical alert. Severe airway obstruction is likely. Use fast-acting medication immediately and contact your healthcare provider or seek emergency care.
Tracking trends matters more than isolated readings. A gradual decline over several days—even within the green zone—can signal deteriorating control and warrant a doctor’s review.
Real-Life Application: A Case Study in Early Detection
Sarah, a 34-year-old teacher with moderate persistent asthma, had been relying solely on symptom-based management. She used her rescue inhaler when wheezing started but often ended up missing work due to sudden attacks.
After her pulmonologist introduced daily peak flow monitoring, Sarah began testing each morning before taking her medications. Within a week, she noticed her readings dropped to 75% of her personal best for three consecutive days—despite feeling fine. Following her asthma action plan, she increased her inhaled corticosteroid dose as instructed.
By catching the decline early, she prevented a full-blown exacerbation. Over the next month, her average peak flow improved by 12%, and she reported zero missed workdays. The objective data gave her confidence and control she hadn’t experienced before.
Frequently Asked Questions
How often should I update my personal best peak flow?
Your personal best should be reassessed every few months if your asthma has changed significantly, or after any major improvement in lung function. Otherwise, re-establish it whenever starting regular monitoring or after a prolonged illness.
Can children use peak flow meters effectively?
Children aged five and older can typically perform the maneuver correctly, though younger kids may struggle with coordination. Supervision and practice are key. For younger children, spirometry in a clinical setting may be more reliable.
Why do my peak flow numbers vary throughout the day?
Daily variation is normal, especially in asthmatics. Peak flow is usually lowest in the early morning and highest in the mid-afternoon. Greater than 20% variability between morning and evening readings suggests poorly controlled asthma.
Essential Checklist for Reliable Monitoring
To ensure every reading counts, follow this checklist before each test:
- ✅ Reset the marker to zero
- ✅ Stand or sit upright
- ✅ Take a full, deep breath
- ✅ Seal lips tightly around the mouthpiece
- ✅ Exhale quickly and forcefully in one burst
- ✅ Record the highest of three attempts
- ✅ Log the result with date, time, and symptoms
Conclusion: Take Control of Your Respiratory Health
Mastering peak flow meter measurements transforms lung monitoring from guesswork into a precise, actionable practice. With consistent technique, accurate devices, and thoughtful interpretation, you gain early warning signals that empower timely decisions. Whether you're managing asthma in yourself or a loved one, this simple tool offers profound benefits when used correctly.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?