Light bleeding or spotting between menstrual periods is more common than many people realize. While it’s often harmless, it can sometimes signal an underlying condition that requires attention. For individuals tracking their reproductive health, unexpected spotting can be confusing—even alarming. Understanding the potential causes, recognizing red flags, and knowing when to consult a healthcare provider are essential steps in managing this experience with confidence.
Unlike full menstrual flow, intermenstrual spotting typically appears as light pink, brown, or red discharge. It may last a few hours or persist for several days. Although occasional spotting isn’t usually cause for alarm, persistent or recurring episodes warrant investigation.
Common Causes of Mid-Cycle Spotting
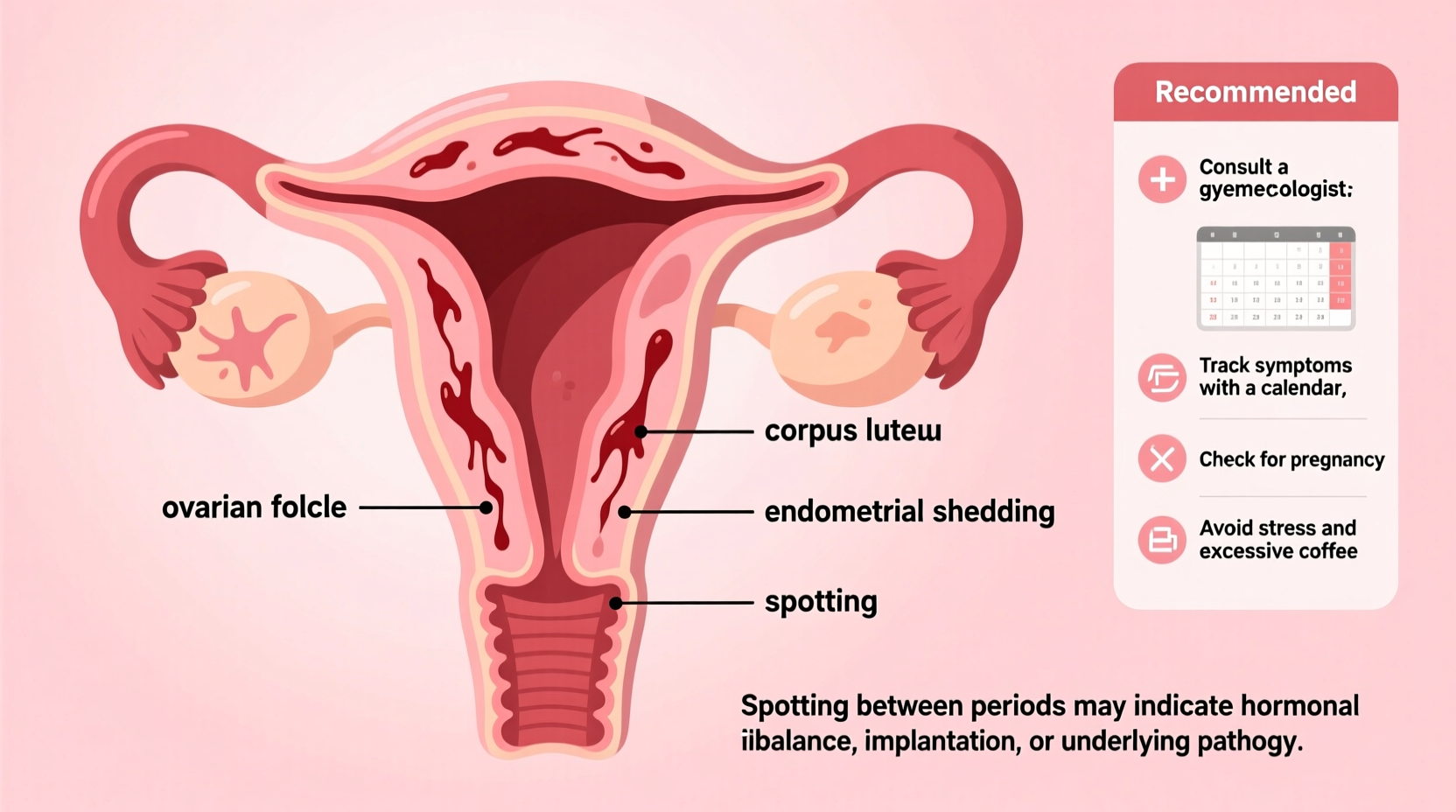
Several physiological and lifestyle-related factors can lead to spotting outside of your regular period. Some are entirely normal; others may point to conditions needing medical evaluation.
- Ovulation: Around day 14 of a typical cycle, some women experience light spotting due to hormonal shifts during ovulation. This is known as \"ovulatory bleeding\" and is usually short-lived.
- Hormonal contraceptives: Birth control pills, implants, IUDs (especially copper or hormonal types), and patches can cause breakthrough bleeding, particularly in the first few months of use.
- Implantation bleeding: In early pregnancy, light spotting may occur when a fertilized egg attaches to the uterine lining—usually about 6–12 days after conception.
- Stress or significant weight changes: Emotional stress, rapid weight loss or gain, and intense exercise can disrupt hormone balance, leading to irregular bleeding.
- Perimenopause: As women approach menopause, fluctuating estrogen levels often result in unpredictable cycles and mid-cycle spotting.
When Spotting May Signal a Medical Condition
While many causes of spotting are benign, certain conditions require diagnosis and treatment. Persistent or heavy intermenstrual bleeding should never be ignored.
- Polycystic Ovary Syndrome (PCOS): Characterized by irregular periods, excess androgen, and ovarian cysts, PCOS often leads to unpredictable bleeding patterns.
- Uterine fibroids or polyps: Noncancerous growths in the uterus can cause spotting, heavier periods, or pelvic pressure.
- Infections: Sexually transmitted infections like chlamydia or gonorrhea can inflame the cervix (cervicitis), resulting in post-coital or intermenstrual bleeding.
- Endometriosis: Tissue similar to the uterine lining grows outside the uterus, potentially causing pain and irregular bleeding.
- Cervical or endometrial cancer: Though less common, abnormal bleeding—especially after menopause or post-sex—is a key symptom requiring immediate evaluation.
“Any unexplained vaginal bleeding, especially if it recurs or worsens, deserves a thorough assessment. Early detection can make a critical difference.” — Dr. Lena Patel, OB-GYN Specialist
Do’s and Don’ts: Managing Spotting Between Periods
| Do’s | Don’ts |
|---|---|
| Track your cycle and note when spotting occurs | Ignore persistent or worsening spotting |
| Use panty liners to manage light discharge | Assume all spotting is “normal” without evaluation |
| Practice safe sex to reduce infection risk | Self-diagnose based on internet searches |
| Schedule a check-up if spotting lasts over two cycles | Delay seeing a doctor if you’re pregnant or trying to conceive |
| Maintain a healthy lifestyle to support hormonal balance | Overuse hormonal supplements without supervision |
Step-by-Step Guide: What to Do If You Experience Spotting
If you notice spotting between periods, follow this practical sequence to determine whether professional care is needed:
- Document the details: Record the date, duration, color, amount (light, medium, heavy), and any associated symptoms such as cramps, fatigue, or dizziness.
- Review recent changes: Consider new medications, birth control, stress levels, travel, or sexual activity that might influence your cycle.
- Take a pregnancy test: Especially if you're sexually active and not using contraception consistently. Implantation bleeding can mimic spotting.
- Monitor for recurrence: One isolated episode may not be concerning. But if spotting happens two or more times in a row, proceed to step five.
- Schedule a gynecological exam: Your provider may perform a pelvic exam, Pap smear, ultrasound, or blood tests to check hormone levels and rule out pathology.
Mini Case Study: Sarah’s Experience with Recurring Spotting
Sarah, a 34-year-old teacher, began noticing light brown discharge about a week after her period ended. At first, she dismissed it as stress-related, but after three consecutive months, she decided to see her gynecologist. An ultrasound revealed a small endometrial polyp. After a minor outpatient procedure to remove it, her cycles normalized. “I wish I hadn’t waited so long,” she said. “It wasn’t painful, but it was unsettling. Now I know: don’t ignore your body’s signals.”
Prevention and Lifestyle Adjustments
While not all causes of spotting can be prevented, certain habits support hormonal stability and reproductive health:
- Balanced nutrition: Diets rich in iron, omega-3 fatty acids, and B vitamins support healthy menstruation.
- Regular sleep patterns: Poor sleep disrupts cortisol and melatonin, which can indirectly affect reproductive hormones.
- Stress reduction: Practices like yoga, meditation, or therapy can mitigate the impact of chronic stress on your cycle.
- Avoid smoking: Tobacco use has been linked to earlier menopause and increased menstrual irregularities.
Frequently Asked Questions
Is spotting between periods always a sign of pregnancy?
No. While implantation bleeding is one possible cause, many non-pregnancy-related factors—including ovulation, stress, or hormonal birth control—can also lead to spotting. A pregnancy test can help clarify the cause.
Can spotting be a sign of cancer?
In rare cases, yes. Abnormal uterine bleeding—especially after menopause or following intercourse—can be an early symptom of cervical or endometrial cancer. However, most cases of intermenstrual bleeding are due to benign causes. Still, any persistent change warrants medical review.
Should I stop using tampons if I’m spotting?
There’s no need to avoid tampons solely because of spotting, but if you're experiencing frequent or unexplained bleeding, switching to pads may help you better monitor the amount and appearance. This information can be useful during a medical consultation.
Conclusion: Take Charge of Your Reproductive Health
Spotting between periods doesn’t automatically mean something is wrong, but it shouldn’t be routinely dismissed either. By paying attention to your body, recording symptoms, and seeking timely medical input, you empower yourself to maintain optimal reproductive wellness. Whether it's adjusting your lifestyle, changing contraception, or addressing an underlying condition, early action leads to better outcomes.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?