Photophobia isn't a fear of light—it's a medical condition characterized by an abnormal intolerance to light. People experiencing it may feel discomfort or pain when exposed to natural sunlight, fluorescent lighting, or even the glow from digital screens. While occasional sensitivity can happen to anyone, persistent or severe reactions often point to underlying health issues. Understanding why you're sensitive to light is the first step toward managing symptoms and improving quality of life.
What Is Photophobia?
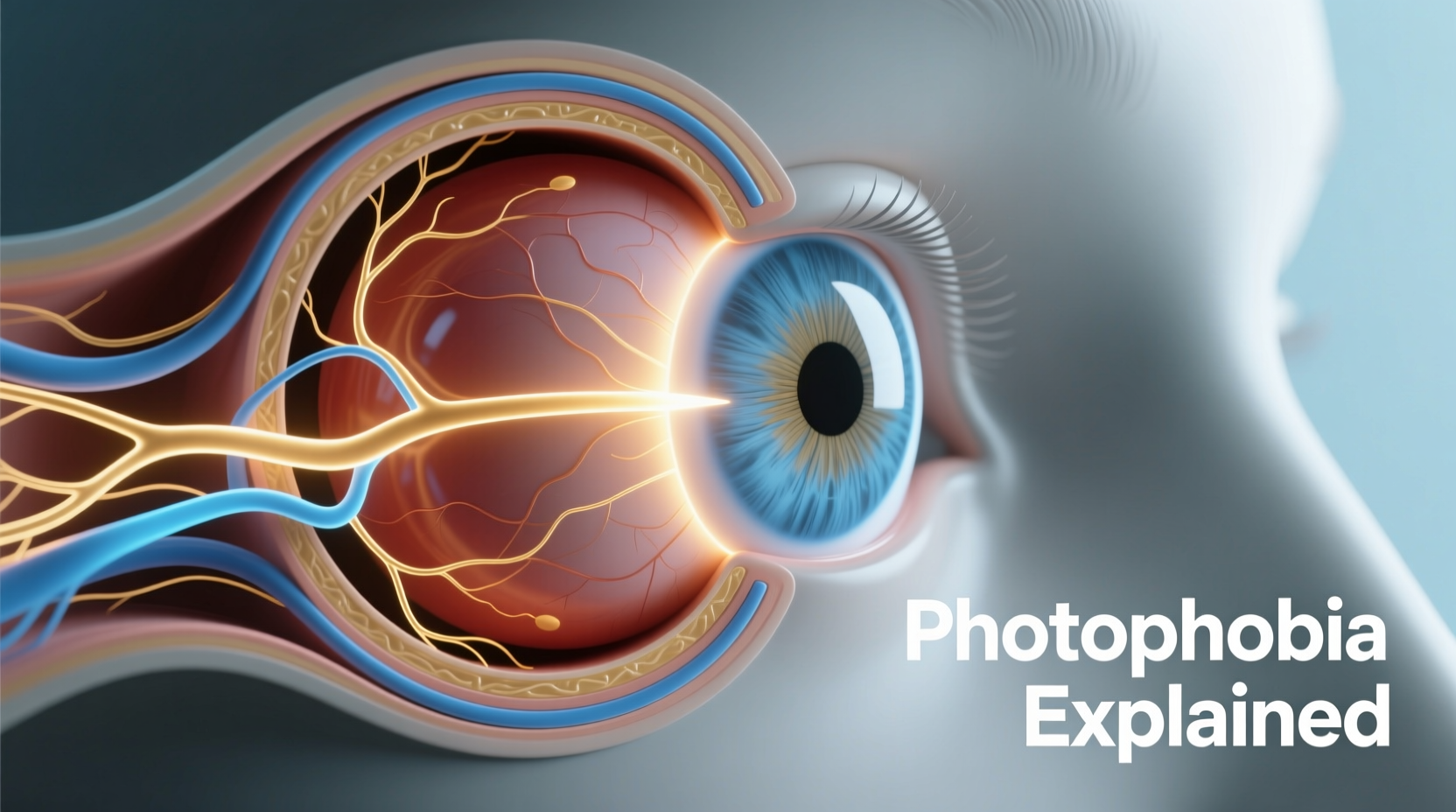
Photophobia refers to an increased sensitivity to light that leads to physical discomfort, eye strain, headaches, or the need to squint or close your eyes in bright environments. It’s not a standalone disease but rather a symptom of other neurological, ocular, or systemic conditions. The severity varies widely: some individuals experience mild irritation under harsh office lighting, while others are forced to stay in darkened rooms during flare-ups.
The brain interprets certain light wavelengths—especially blue light from screens and LED bulbs—as overwhelming signals when neural pathways are disrupted. This misfiring can originate in the retina, optic nerve, or regions of the brain responsible for processing visual stimuli.
“Photophobia is more than just discomfort—it’s a neurological response indicating that something in the visual or central nervous system is off-balance.” — Dr. Lena Torres, Neuro-Ophthalmologist, Massachusetts Eye & Ear
Common Causes of Light Sensitivity
Light sensitivity rarely occurs in isolation. It usually accompanies another condition. Identifying the root cause is essential for effective treatment.
- Migraines: Over 80% of migraine sufferers report photophobia during attacks. Light can intensify headache pain and prolong episodes.
- Dry Eye Syndrome: Insufficient tear production makes the cornea more vulnerable to irritation from bright light.
- Concussions and Traumatic Brain Injuries (TBI): Damage to the brain’s visual processing centers can heighten light sensitivity for weeks or months post-injury.
- Uveitis and Other Eye Inflammations: Inflammation inside the eye increases vulnerability to light exposure.
- Corneal Abrasions or Infections: Surface damage on the eye amplifies discomfort when light hits the injured area.
- Medications: Certain drugs—including tetracycline antibiotics, antihistamines, and some antidepressants—can increase photosensitivity as a side effect.
- Neurological Disorders: Conditions like meningitis, epilepsy, and multiple sclerosis may involve photophobic symptoms due to altered brain signaling.
- Autoimmune Diseases: Lupus and Sjögren’s syndrome sometimes manifest with ocular dryness and light intolerance.
Triggers That Worsen Photophobia
Even if the underlying condition is stable, everyday environmental factors can trigger or worsen symptoms. Recognizing these can help you avoid unnecessary discomfort.
| Trigger | Why It Affects You | How to Reduce Exposure |
|---|---|---|
| Fluorescent Lighting | Emits flicker and high levels of blue spectrum light | Use desk lamps with warm LEDs; request workplace accommodations |
| Computer and Phone Screens | Blue light strains over-sensitive retinas and disrupts circadian rhythms | Enable night mode; use blue-light-blocking glasses |
| Bright Sunlight | UV and intense visible light overwhelm the optic nerves | Wear wraparound UV-protective sunglasses outdoors |
| LED Headlights at Night | High-intensity beams create glare and halos for sensitive eyes | Adjust driving times; consider anti-glare lenses |
Diagnosis and When to Seek Help
If light sensitivity interferes with daily activities—such as working, reading, or commuting—it should be evaluated by a healthcare provider. Diagnosis typically involves a multidisciplinary approach:
- Ophthalmological Exam: An eye specialist checks for structural issues like corneal damage, cataracts, or inflammation.
- Neurological Assessment: For cases linked to migraines or head injuries, neuroimaging (MRI or CT scans) may be recommended.
- Patient History Review: Doctors analyze patterns—when symptoms occur, duration, associated symptoms (headaches, nausea), and potential triggers.
Sudden onset of photophobia with fever, neck stiffness, or confusion could indicate meningitis—a medical emergency requiring immediate attention.
Mini Case Study: Recovering from Post-Concussion Photophobia
Sarah, a 28-year-old graphic designer, developed severe light sensitivity after slipping on ice and hitting her head. Initially dismissed as “just a bump,” she struggled to work under office lighting and experienced daily headaches. After three weeks of worsening symptoms, she saw a neurologist who diagnosed post-concussion syndrome. Her treatment included cognitive rest, gradual screen reintroduction, wearing FL-41 tinted glasses indoors, and vestibular therapy. Within two months, her tolerance improved significantly, allowing her to return to full-time work with modified lighting setups.
Managing and Reducing Light Sensitivity
While treating the underlying cause is paramount, several strategies can reduce day-to-day discomfort and prevent flare-ups.
Step-by-Step Guide to Managing Photophobia
- Track Your Symptoms: Keep a journal noting when sensitivity occurs, intensity level, location, and possible triggers (e.g., screen time, weather changes).
- Optimize Indoor Lighting: Replace fluorescent bulbs with warm-white LEDs (2700K–3000K). Use dimmer switches and indirect lighting.
- Wear Protective Eyewear: Choose sunglasses with 100% UVA/UVB protection. Consider specialized tints like FL-41, proven to reduce migraine-related photophobia.
- Adjust Digital Devices: Lower screen brightness, enable dark mode, and use software like f.lux to reduce blue light emission at night.
- Create Low-Light Zones: Designate a rest area at home with blackout curtains and minimal artificial lighting for recovery during flare-ups.
- Stay Hydrated and Rested: Dehydration and fatigue lower your threshold for sensory overload, including light sensitivity.
Checklist: Daily Habits to Reduce Photophobia Flare-Ups
- ☑ Wear blue-light-filtering glasses during screen use
- ☑ Avoid overhead fluorescent lights at work or home
- ☑ Take regular breaks using the 20-20-20 rule (every 20 minutes, look at something 20 feet away for 20 seconds)
- ☑ Use matte screen protectors to reduce glare
- ☑ Carry polarized sunglasses for outdoor exposure
- ☑ Maintain consistent sleep schedule to support neurological stability
Frequently Asked Questions
Can photophobia go away on its own?
In temporary cases—such as those caused by minor eye strain or short-term medication use—photophobia may resolve once the trigger is removed. However, chronic photophobia related to migraines, brain injury, or autoimmune disorders often requires ongoing management and does not typically disappear without intervention.
Are children susceptible to photophobia?
Yes. Children with migraines, autism spectrum disorder, or developmental delays often exhibit light sensitivity. Parents might notice them avoiding brightly lit classrooms, covering their eyes, or complaining of headaches after screen time. Early evaluation can lead to better academic performance and comfort.
Is there a test specifically for photophobia?
There is no single diagnostic test, but clinicians use tools like the Acute Photophobia Scale and functional imaging studies to assess severity. Diagnosis relies heavily on patient-reported experiences combined with clinical findings.
Conclusion: Taking Control of Your Light Sensitivity
Understanding why you're sensitive to light empowers you to take meaningful steps toward relief. Whether your photophobia stems from migraines, eye health issues, or neurological changes, identifying triggers and implementing protective habits can dramatically improve your daily function. Don’t dismiss persistent sensitivity as normal—it’s your body signaling that something needs attention. With proper diagnosis, lifestyle adjustments, and professional support, many people regain comfort in environments they once had to avoid.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?