Tonsils are small but powerful organs located at the back of the throat, often dismissed as unnecessary or even problematic. Yet, they play a critical role in immune defense—especially during early development. Despite their importance, many people undergo tonsillectomy each year due to chronic infections or obstructive conditions. Understanding why tonsils exist, how they contribute to health, and under what circumstances they should be removed can help individuals make informed medical decisions.
The Immune Role of Tonsils: More Than Just Lumps of Tissue
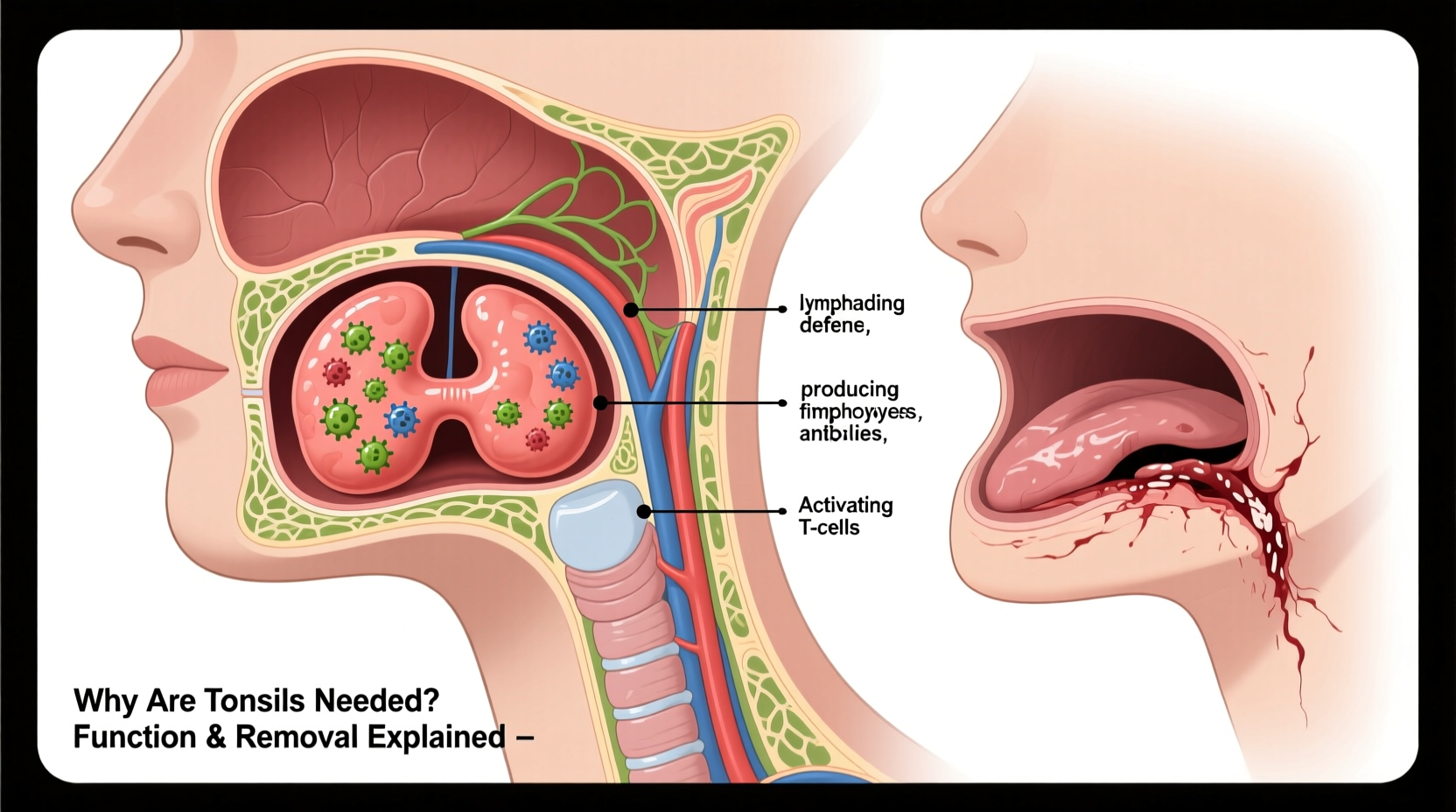
Tonsils are part of the lymphatic system and act as the body’s first line of defense against pathogens entering through the mouth and nose. Positioned strategically on either side of the throat (palatine tonsils), along with adenoids and lingual tonsils, they form a ring of immune tissue known as Waldeyer’s ring.
When viruses or bacteria enter the respiratory tract, the tonsils sample these invaders and initiate an immune response. They contain specialized white blood cells that produce antibodies and activate other immune defenses. This surveillance system is particularly active in children, whose immune systems are still developing.
“Tonsils serve as sentinels of the immune system, especially in early life. Their activity helps train the body to recognize and respond to common pathogens.” — Dr. Lena Patel, Pediatric Immunologist
In infants and young children, the tonsils are proportionally larger and more active. As we age, their immune function diminishes, and other parts of the lymphatic system take over. However, this does not mean they become useless; they continue to monitor incoming threats throughout adulthood, albeit less prominently.
When Tonsils Become a Problem: Indications for Removal
Despite their protective role, tonsils can sometimes cause more harm than good. When they become chronically infected or enlarged, they may compromise breathing, swallowing, or overall quality of life. The decision to remove them—through a procedure called tonsillectomy—is based on clinical evidence and patient history.
Common reasons for tonsil removal include:
- Recurrent tonsillitis: Seven or more episodes in one year, five per year for two consecutive years, or three per year for three years.
- Obstructive sleep apnea: Enlarged tonsils block the airway during sleep, leading to snoring, gasping, or interrupted breathing.
- Peritonsillar abscess: A severe infection that forms around the tonsil, potentially spreading if untreated.
- Dysphagia: Difficulty swallowing due to significant enlargement.
- Suspected malignancy: Rarely, abnormal growths in the tonsil tissue require surgical evaluation.
Comparing Conservative Care vs. Surgical Intervention
| Approach | Benefits | Risks/Limitations |
|---|---|---|
| Antibiotics & Pain Management | Avoids surgery; effective for bacterial infections | Does not prevent recurrence; antibiotic resistance possible |
| Tonsillectomy | Reduces infection frequency; improves sleep and breathing | Surgical risks; recovery period of 7–14 days; bleeding risk |
| Watchful Waiting | Allows time to assess severity; avoids unnecessary procedures | May delay relief for those with severe symptoms |
The choice between managing tonsil issues conservatively versus opting for surgery depends on the frequency and impact of symptoms. For some, occasional sore throats are manageable. For others, repeated illness leads to missed school, poor sleep, and declining well-being—making surgery a reasonable option.
Real-Life Example: A Child Regains Restful Sleep
Eight-year-old Marcus had been snoring loudly for over a year. His parents noticed he frequently stopped breathing during sleep and woke up tired despite going to bed early. He struggled to focus in class and was often irritable. After a sleep study confirmed moderate obstructive sleep apnea caused by enlarged tonsils, his ENT specialist recommended a tonsillectomy.
Within two weeks of surgery, Marcus’s breathing normalized. His snoring disappeared, and his energy levels improved dramatically. Teachers reported better concentration, and his parents noted a positive shift in mood and daytime alertness. While recovery involved a week of soft foods and pain management, the long-term benefits far outweighed the temporary discomfort.
What Happens During and After a Tonsillectomy?
A tonsillectomy is typically performed under general anesthesia and takes about 30 minutes. Surgeons use various techniques—including cauterization, harmonic scalpel, or cold knife dissection—to remove the tonsils. Most patients go home the same day, though young children or those with complications may stay overnight.
Post-Surgery Recovery Timeline
- Days 1–3: Significant throat pain; limited eating; prescribed pain medication required.
- Days 4–7: Pain begins to subside; gradual return to soft foods like yogurt, applesauce, and mashed potatoes.
- Days 8–10: Scabs begin to slough off—a normal process that carries a small risk of bleeding.
- Day 14 onward: Most adults and children feel fully recovered, though fatigue may linger slightly.
Bleeding is the most serious postoperative complication, occurring in about 2–5% of cases, usually around days 7–10. Immediate medical attention is required if bright red blood appears in saliva or vomit.
Frequently Asked Questions
Will removing tonsils weaken my immune system?
No conclusive evidence shows that tonsillectomy significantly impairs long-term immunity. Other lymphoid tissues compensate for the loss, and most patients experience fewer infections after surgery due to the elimination of a persistent source of inflammation.
Can tonsils grow back after removal?
Complete regrowth is rare, but partial tissue regeneration can occur if remnants are left behind. This doesn’t usually cause clinical problems and is more common in younger children.
Is tonsillectomy only for children?
No. Adults also undergo the procedure, often for chronic tonsillitis or sleep apnea. Recovery may be more painful and prolonged in adults due to denser tissue and higher pain sensitivity.
Conclusion: Balancing Function and Necessity
Tonsils serve a valuable purpose in immune surveillance, particularly during childhood. They are not redundant organs but rather specialized defenders at the gateway of the respiratory and digestive tracts. However, when their presence leads to recurrent illness, breathing difficulties, or disrupted sleep, removal becomes a medically sound decision.
Modern medicine emphasizes individualized care—weighing the benefits of retention against the burdens of disease. With proper diagnosis and thoughtful discussion between patients, families, and healthcare providers, the decision to keep or remove tonsils can be made with confidence and clarity.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?