Difficulty breathing through the nose is a surprisingly common issue that affects millions of people daily. Whether it's a temporary blockage from a cold or a chronic structural problem, nasal obstruction can disrupt sleep, reduce oxygen intake, impair concentration, and diminish quality of life. While many assume it’s just “a stuffy nose,” the underlying causes vary widely — from allergies and infections to anatomical irregularities. Understanding what’s truly blocking your airflow is the first step toward lasting relief.
Common Causes of Nasal Obstruction
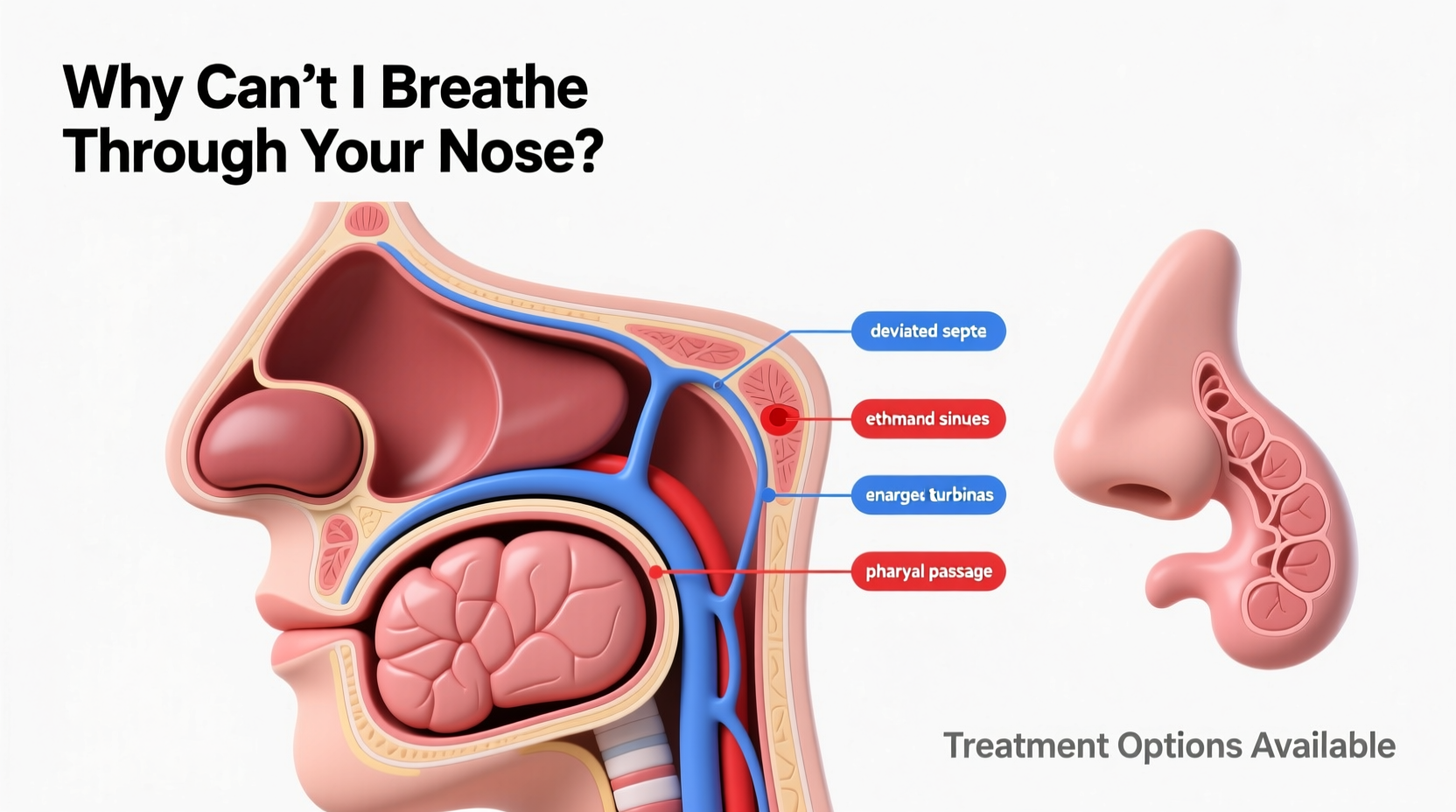
Nasal congestion isn’t always due to mucus buildup. The inability to breathe through the nose can stem from inflammation, physical blockages, or neurological factors affecting blood flow in nasal tissues. Below are the most frequent culprits:
- Allergic rhinitis: Exposure to allergens like pollen, dust mites, or pet dander triggers immune responses that inflame nasal passages.
- Viral infections: Colds and flu cause swelling of the nasal mucosa and increased mucus production.
- Sinusitis: Acute or chronic sinus infections lead to thick mucus and pressure buildup around the nasal cavity.
- Deviated septum: A crooked nasal septum (the wall between nostrils) can obstruct one or both sides of the nasal passage.
- Nasal polyps: Soft, noncancerous growths in the lining of the nose or sinuses can block airflow over time.
- Enlarged turbinates: Turbinates are bony structures inside the nose that humidify air; they can swell chronically due to irritation or anatomy.
- Medication-induced rhinitis: Overuse of nasal decongestant sprays (like oxymetazoline) can worsen congestion—a condition known as rebound rhinitis.
- Hormonal changes: Pregnancy, menstruation, or thyroid disorders may increase nasal tissue sensitivity and swelling.
Treatment Options Based on Cause
Effective treatment depends entirely on identifying the root cause. Self-treating with over-the-counter remedies may provide short-term relief but often fails to resolve chronic issues.
Allergies and Inflammation
For allergy-related congestion, antihistamines (such as loratadine or cetirizine), intranasal corticosteroids (like fluticasone), and leukotriene inhibitors (montelukast) are commonly prescribed. Avoiding allergens through air filtration and environmental control also plays a critical role.
Infections
Viral infections typically resolve within a week. Supportive care includes saline rinses, hydration, rest, and pain relievers. Bacterial sinusitis may require antibiotics if symptoms persist beyond 10 days or worsen after initial improvement.
Anatomical Issues
Structural problems such as a deviated septum or nasal polyps often don’t respond well to medication alone. Surgical interventions like septoplasty (to straighten the septum) or endoscopic sinus surgery (to remove polyps) may be necessary for long-term relief.
“Chronic nasal obstruction impacts not only breathing but also sleep quality, voice resonance, and even dental health due to mouth-breathing.” — Dr. Alan Wu, Otolaryngologist at Massachusetts Eye and Ear
Do’s and Don’ts: Managing Nasal Congestion
| Action | Recommendation |
|---|---|
| Use saline nasal spray | DO: Helps moisturize dry passages and flush irritants |
| Take oral decongestants | USE CAUTIOUSLY: Can raise blood pressure; avoid if hypertensive |
| Use nasal decongestant sprays | DON’T: Limit use to 3 days max to prevent rebound congestion |
| Try neti pots | DO: Use sterile or distilled water only—never tap water |
| Smoke or expose yourself to secondhand smoke | DON’T: Smoke irritates nasal membranes and worsens inflammation |
| Ignore persistent symptoms | SEEK HELP: Chronic congestion could indicate polyps or other conditions needing evaluation |
Step-by-Step Guide to Regaining Nasal Breathing
- Assess symptom duration: Is the issue acute (less than 4 weeks) or chronic (more than 12 weeks)? This helps determine whether infection, allergy, or structure is likely responsible.
- Track triggers: Note patterns—do symptoms flare during pollen season, after dust exposure, or at night? Keeping a symptom diary can reveal hidden allergens or irritants.
- Start conservative treatment: Begin with daily saline irrigation and a steroid nasal spray for two weeks. These are safe for long-term use and effective for many causes.
- Evaluate response: If no improvement occurs, consult a healthcare provider. They may recommend allergy testing, imaging (CT scan), or nasal endoscopy.
- Consider specialty care: An otolaryngologist (ENT) can diagnose structural issues and discuss surgical options if appropriate.
Real-Life Example: Sarah’s Journey to Clearer Breathing
Sarah, a 34-year-old teacher, struggled with year-round nasal congestion. She assumed it was seasonal allergies and used OTC antihistamines and decongestants regularly. Despite this, she woke up exhausted, snored loudly, and relied on mouth breathing. After six months of disrupted sleep, she visited an ENT specialist. A nasal endoscopy revealed large nasal polyps and a moderate septal deviation. She underwent outpatient endoscopic sinus surgery to remove the polyps and had her septum corrected. Within three weeks, her breathing improved dramatically. Follow-up care included steroid rinses and allergen avoidance strategies. Today, Sarah sleeps better, has more energy, and rarely uses medication.
When to See a Doctor
While occasional congestion is normal, certain red flags warrant medical attention:
- One-sided nasal blockage that doesn’t change with position
- Persistent loss of smell lasting more than two weeks
- Frequent nosebleeds or facial numbness
- Green or foul-smelling nasal discharge
- Swelling around the eyes or forehead pain with fever
These symptoms may indicate serious conditions such as fungal sinusitis, tumors, or complications requiring urgent intervention.
FAQ
Can anxiety make me feel like I can’t breathe through my nose?
Yes. While anxiety doesn’t physically block nasal passages, it can alter breathing perception. Hyperventilation or chest tightness may create a sensation of nasal obstruction even when airflow is normal. Breathing exercises and mindfulness techniques often help alleviate these symptoms.
Is it bad to breathe through my mouth all the time?
Chronic mouth breathing, especially in children, can lead to dental misalignment, dry mouth, increased risk of respiratory infections, and poor sleep quality. In adults, it contributes to snoring, gum disease, and fatigue. Restoring nasal breathing should be a priority for overall health.
Are nasal strips effective for long-term use?
Nasal strips (like Breathe Right) can help open nasal valves during exercise or sleep, particularly in people with mild valve collapse. However, they offer only temporary support and don’t treat underlying causes like polyps or chronic inflammation.
Conclusion: Take Control of Your Breathing
Not being able to breathe through your nose is more than an inconvenience—it can affect your sleep, immunity, focus, and emotional well-being. The good news is that most causes are diagnosable and treatable. From simple lifestyle adjustments and medications to advanced procedures, solutions exist for nearly every case. Don’t accept chronic congestion as normal. Identify your triggers, try evidence-based treatments, and seek expert care when needed. Your ability to breathe freely is not just a comfort—it’s a cornerstone of health.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?