Struggling to fully empty your bladder is more than just a minor inconvenience—it can lead to discomfort, recurrent infections, and long-term complications if left unaddressed. This condition, known medically as urinary retention or incomplete bladder emptying, affects both men and women across various age groups. While occasional difficulty may not be alarming, persistent symptoms should never be ignored. Understanding the underlying causes and adopting effective management strategies can significantly improve quality of life.
Common Causes of Incomplete Bladder Emptying
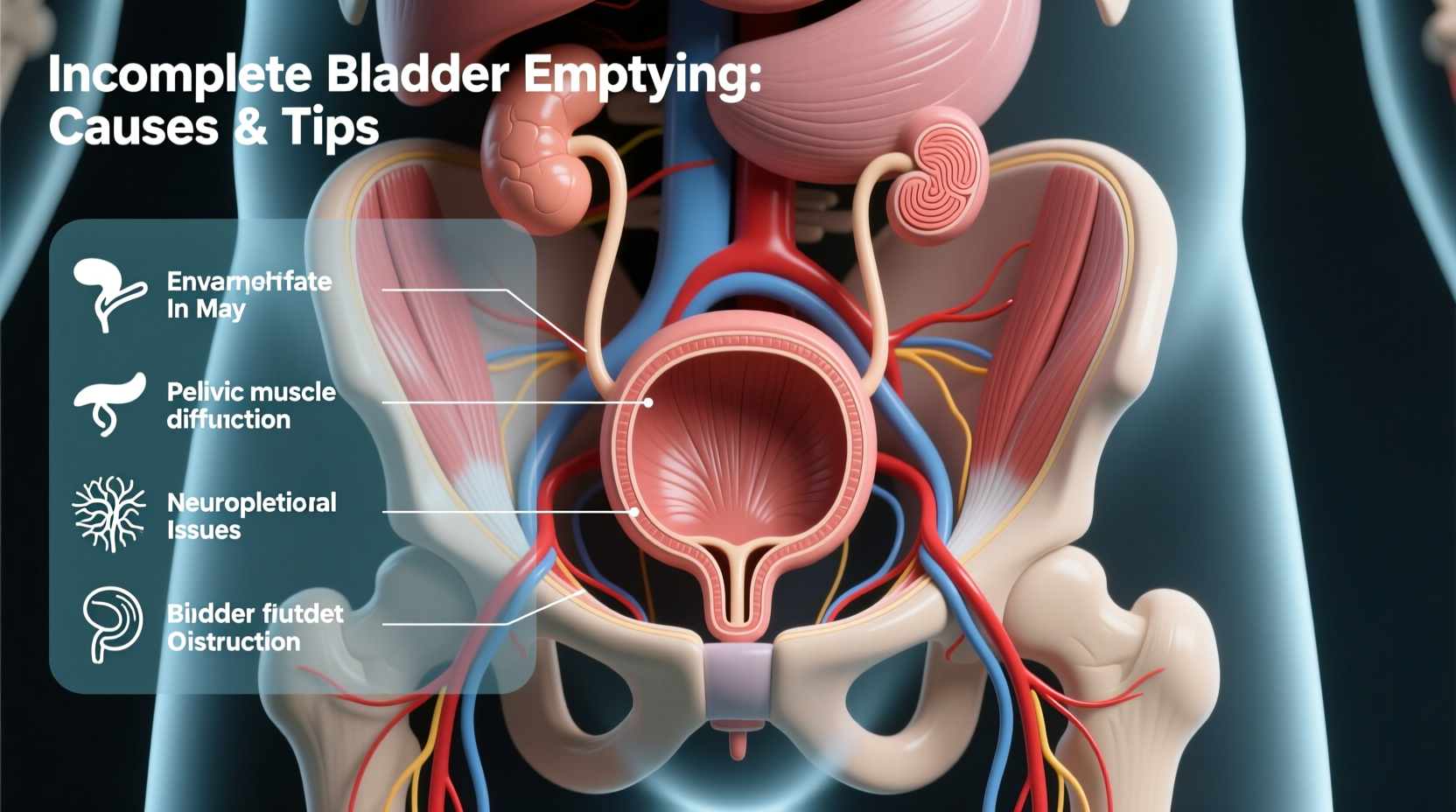
Inability to fully void the bladder stems from a range of physiological, neurological, and lifestyle-related factors. Identifying the root cause is essential for appropriate treatment.
- Benign Prostatic Hyperplasia (BPH): In men, an enlarged prostate is one of the most frequent causes. As the prostate grows with age, it can press against the urethra, restricting urine flow.
- Neurological Disorders: Conditions like multiple sclerosis, Parkinson’s disease, stroke, or spinal cord injuries can disrupt nerve signals between the brain and bladder, impairing coordination.
- Bladder Muscle Weakness: The detrusor muscle, responsible for contracting the bladder, may weaken due to aging, surgery, or chronic overdistension.
- Urinary Tract Obstructions: Kidney stones, tumors, or strictures in the urethra can physically block urine passage.
- Medications: Antihistamines, decongestants, antidepressants, and certain antipsychotics can interfere with bladder contraction or increase sphincter resistance.
- Pelvic Floor Dysfunction: In women, especially after childbirth or pelvic surgery, weakened or overly tight pelvic floor muscles can hinder proper bladder emptying.
- Diabetes: Long-term high blood sugar levels can damage nerves that control bladder function—a condition called diabetic cystopathy.
Recognizing the Symptoms
Many people dismiss mild urinary hesitancy or frequency as normal aging, but early signs of incomplete voiding include:
- Feeling the need to urinate again shortly after finishing
- Dribbling after urination
- Weak or interrupted urine stream
- Straining to start or maintain urination
- Sensation of fullness even after going to the bathroom
- Recurrent urinary tract infections (UTIs)
Left untreated, residual urine in the bladder creates a breeding ground for bacteria, increasing the risk of UTIs and potentially leading to kidney damage.
Practical Tips to Improve Bladder Emptying
While medical intervention may be necessary depending on the cause, several lifestyle and behavioral adjustments can support better bladder function.
- Double Voiding Technique: After urinating, wait a few seconds, then try again. This helps ensure the bladder empties more completely by allowing time for additional urine to drain.
- Lean Forward While Urinating: Sitting upright and leaning slightly forward can enhance bladder contraction and reduce post-void residual volume.
- Avoid Holding Urine: Delaying urination regularly stretches the bladder beyond its optimal capacity, weakening the muscle over time.
- Stay Hydrated—but Wisely: Drink adequate water throughout the day, but reduce intake two hours before bedtime to minimize nighttime urges without causing dehydration.
- Limit Bladder Irritants: Caffeine, alcohol, carbonated drinks, and spicy foods can aggravate bladder sensitivity and worsen symptoms.
- Practice Pelvic Floor Exercises: For those with weak pelvic support, Kegel exercises strengthen the muscles involved in bladder control. However, if the muscles are too tight, relaxation techniques may be needed instead.
| Action | Benefit | Frequency/Duration |
|---|---|---|
| Double voiding | Reduces residual urine | After every bathroom visit |
| Kegel exercises | Strengthens pelvic floor | 3 sets of 10 daily |
| Timed voiding | Prevents overfilling | Every 2–3 hours during day |
| Fluid management | Controls urgency | Evenly spaced intake |
When to See a Doctor: A Real-Life Example
Consider James, a 58-year-old office worker who began noticing he had to go to the bathroom frequently at night. He assumed it was due to drinking coffee late in the day. Over several months, however, his symptoms worsened—he often felt pressure in his lower abdomen and occasionally leaked urine. During a routine check-up, his physician performed a post-void residual (PVR) test using ultrasound and discovered over 300 mL of urine remaining after voiding (normal is less than 50 mL). Further evaluation revealed moderate BPH. With medication and lifestyle changes, James saw significant improvement within six weeks.
This case illustrates how seemingly minor symptoms can signal a larger issue—and why early assessment matters.
“Patients often wait too long to seek help for urinary symptoms. But timely diagnosis can prevent complications like bladder damage or kidney issues.” — Dr. Lena Torres, Urologist, Cleveland Clinic
Medical Evaluation and Treatment Options
If self-management doesn’t relieve symptoms, a healthcare provider may recommend diagnostic tests such as:
- Post-void residual (PVR) measurement: Uses ultrasound or catheterization to assess how much urine remains after urination.
- Uroflowmetry: Measures the speed and volume of urine flow.
- Cystoscopy: A thin scope examines the urethra and bladder lining.
- Urodynamic testing: Evaluates bladder pressure and muscle function during filling and voiding.
Treatment depends on the diagnosis:
- Medications: Alpha-blockers (e.g., tamsulosin) relax prostate and bladder neck muscles; 5-alpha reductase inhibitors shrink the prostate over time.
- Catheterization: Intermittent self-catheterization may be recommended for severe retention, especially when surgery isn’t immediate.
- Surgery: Transurethral resection of the prostate (TURP) or laser procedures can relieve obstruction in men with BPH.
- Physical Therapy: Biofeedback and guided pelvic floor therapy benefit those with muscle coordination issues.
Frequently Asked Questions
Can women experience incomplete bladder emptying too?
Yes. While prostate issues are male-specific, women can develop this condition due to pelvic organ prolapse, nerve damage, or pelvic floor dysfunction. Childbirth and hysterectomy are common contributing factors.
Is it dangerous to have leftover urine in the bladder?
Consistently high post-void residuals increase the risk of urinary tract infections, bladder stones, and, in severe cases, kidney damage due to backflow of urine (hydronephrosis).
Are there natural remedies that help?
Some herbal supplements like saw palmetto are used for BPH, but evidence is mixed. Always discuss supplements with your doctor, as they may interact with medications. Behavioral strategies—like double voiding and fluid timing—are among the safest and most effective non-drug approaches.
Take Action for Better Bladder Health
Ignoring persistent urinary symptoms can lead to avoidable health setbacks. Whether it's adjusting habits, strengthening pelvic muscles, or seeking medical evaluation, small steps today can preserve long-term bladder function. Don’t normalize discomfort—your body is signaling for attention. Start tracking your symptoms, apply the tips outlined here, and schedule a consultation if improvements don’t occur within a few weeks.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?