Tumors are abnormal masses of tissue that form when cells divide and grow uncontrollably. While not all tumors are cancerous, their development signals a breakdown in the body’s finely tuned regulation of cell life cycles. Understanding why cells form tumors is essential for early detection, prevention, and treatment. At the core of tumor formation lie two fundamental biological failures: genetic mutations that disrupt normal cell behavior and a compromised immune system that fails to eliminate rogue cells. These two mechanisms work independently or together to allow damaged cells to survive, multiply, and accumulate into detectable growths.
Genetic Mutations: The Internal Trigger
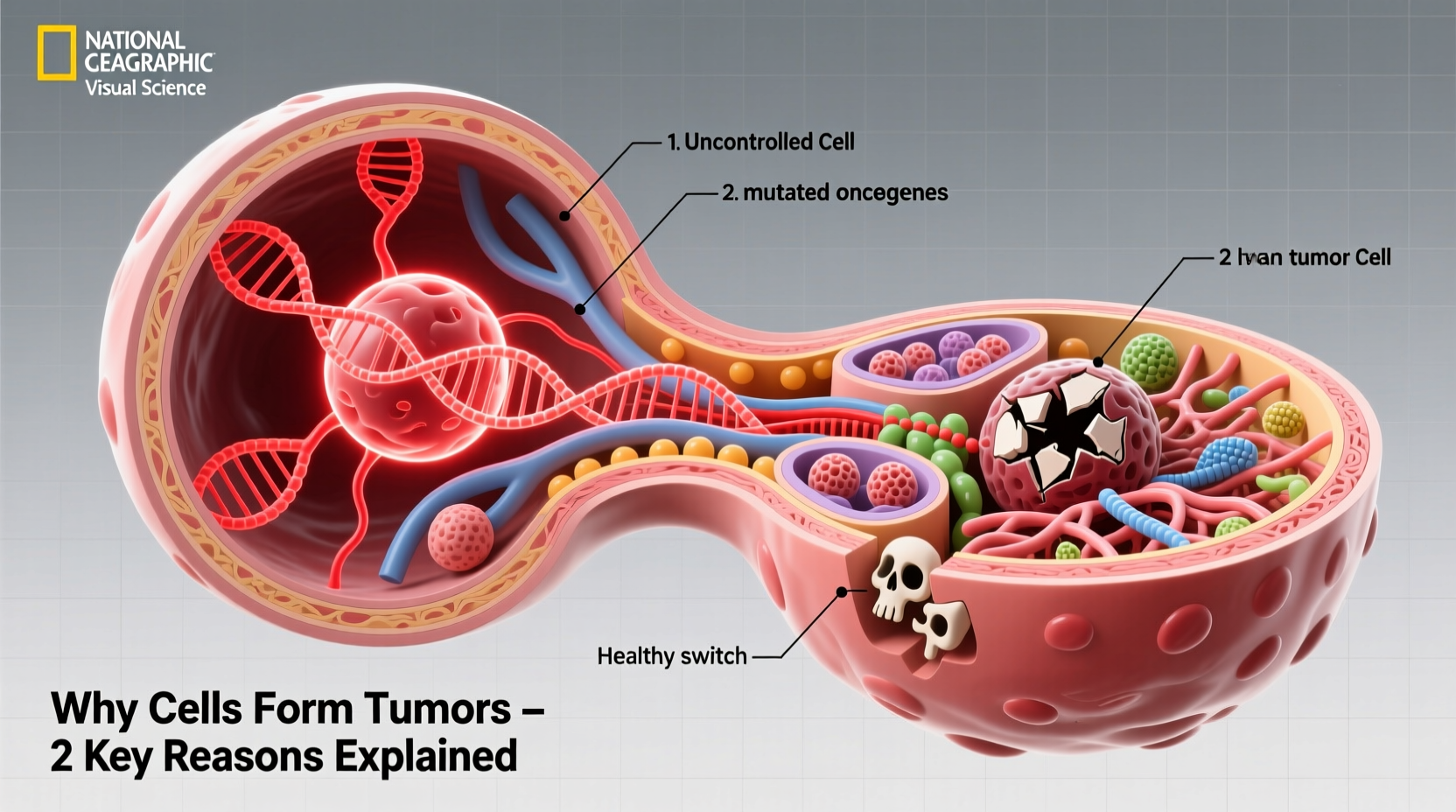
At the most basic level, tumor formation begins with changes in DNA—specifically, mutations in genes that regulate cell division, repair, and death. Every human cell contains thousands of genes that function like switches, turning processes on or off to maintain balance. When these genetic controls fail due to mutation, cells can begin dividing without restraint.
Three main categories of genes are typically involved:
- Oncogenes: Normally involved in promoting cell growth, but when mutated, they become permanently \"on,\" driving excessive division.
- Tumor suppressor genes: These act as brakes on cell division. When inactivated by mutation (e.g., p53 or BRCA1), the brakes fail.
- DNA repair genes: Responsible for fixing errors during replication. If defective, mutations accumulate faster than they can be corrected.
Mutations can arise from various sources: inherited predispositions, environmental exposures (like UV radiation or tobacco), or random errors during DNA replication. Over time, multiple mutations may accumulate in a single cell lineage, progressively pushing it toward malignancy.
“Cancer is fundamentally a disease of the genome. Most tumors harbor dozens to hundreds of mutations, but only a handful drive the process.” — Dr. Bert Vogelstein, Oncologist and Geneticist, Johns Hopkins University
Immune Surveillance Failure: The External Breakdown
The body has a sophisticated defense system designed to detect and destroy abnormal cells before they become problematic. Immune cells, particularly T-cells and natural killer (NK) cells, patrol tissues looking for signs of cellular stress, infection, or mutation. This process is known as immune surveillance.
However, when this system falters—due to age, chronic inflammation, immunosuppressive conditions, or tumor-evolved evasion tactics—abnormal cells can slip through undetected. Some tumors even create microenvironments that actively suppress immune responses, effectively hiding in plain sight.
In fact, one reason older adults face higher cancer rates is immunosenescence—the gradual decline of immune function with age. Similarly, people on long-term immunosuppressants (e.g., organ transplant recipients) have a significantly increased risk of developing tumors.
How Tumors Evade Immune Detection
- Downregulating surface markers that signal “abnormal” to immune cells.
- Secreting chemicals like TGF-beta or IL-10 that dampen immune activity.
- Recruiting regulatory T-cells (Tregs) that protect the tumor instead of attacking it.
- Creating physical barriers such as dense stroma that block immune infiltration.
Synergy Between Mutations and Immune Escape
While either mechanism alone can contribute to tumor formation, the most aggressive cancers usually involve both: a cell acquires mutations that make it hyper-proliferative, then develops strategies to avoid immune destruction. This dual advantage allows it to expand rapidly and resist early elimination.
For example, a lung cell exposed to cigarette smoke may develop a KRAS oncogene mutation, prompting rapid division. If additional mutations disable its ability to display antigenic proteins, cytotoxic T-cells won’t recognize it as a threat. The clone grows unchecked, forming a nodule visible on imaging—a tumor now established.
| Mechanism | Biological Impact | Common Causes |
|---|---|---|
| Genetic Mutations | Uncontrolled cell division, resistance to death signals | Radiation, chemicals, inherited defects, replication errors |
| Immune System Failure | Failure to detect or destroy abnormal cells | Aging, chronic illness, immunosuppressive drugs, tumor evasion tactics |
Real-World Example: Melanoma Development
Consider the case of Sarah, a 48-year-old woman who spent years sunbathing without protection. By her mid-40s, she noticed a mole on her shoulder changing shape and color. A biopsy revealed malignant melanoma.
Genetic testing showed a BRAF V600E mutation—an oncogenic driver common in skin cancers caused by UV damage. This mutation kept her skin cells dividing nonstop. But equally important, analysis of the tumor microenvironment revealed few infiltrating T-cells and high levels of PD-L1 expression, a protein tumors use to deactivate approaching immune cells.
In Sarah’s case, both key factors were at play: a DNA mutation initiated the tumor, and immune evasion allowed it to grow large enough to be diagnosed. Her treatment plan included a BRAF inhibitor to target the mutation and pembrolizumab, an immunotherapy that blocks PD-1/PD-L1 interaction, reactivating her immune system against the cancer.
Actionable Prevention Checklist
You can't control every factor, but you can reduce your risk by focusing on what's within reach. Use this checklist to support cellular health and immune integrity:
- ✅ Avoid tobacco and limit alcohol consumption
- ✅ Wear broad-spectrum sunscreen daily (SPF 30+)
- ✅ Eat a diet rich in antioxidants (berries, leafy greens, nuts)
- ✅ Exercise regularly to boost immune circulation and reduce inflammation
- ✅ Get recommended cancer screenings (e.g., colonoscopy, mammogram, skin checks)
- ✅ Manage chronic conditions like diabetes and obesity, which impair immunity
- ✅ Consider genetic counseling if you have a strong family history of cancer
Frequently Asked Questions
Are all tumors caused by genetic mutations?
Essentially, yes. While external factors like viruses or inflammation can promote tumor growth, nearly all tumors originate from accumulated DNA changes in individual cells. Not all mutations are inherited—most occur during life due to environmental or random causes.
Can a healthy immune system prevent tumors completely?
No system is perfect. Even robust immune defenses miss some abnormal cells. However, a well-functioning immune system greatly reduces the likelihood that precancerous cells will progress to full-blown tumors. Immunocompetent individuals clear potentially dangerous clones more efficiently.
Do benign tumors involve the same mechanisms?
Benign tumors often result from similar mutations but lack the ability to invade nearby tissues or spread. They may not evade immunity as effectively or may have fewer driver mutations. Still, some benign growths can turn malignant over time if additional mutations occur.
Conclusion: Knowledge Is Preventive Power
Understanding why cells form tumors isn’t just academic—it empowers you to make informed choices about lifestyle, screening, and prevention. The two key reasons—genetic instability and immune escape—are interconnected vulnerabilities that modern medicine is learning to address through precision oncology and immunotherapy.
By minimizing mutagen exposure and supporting immune resilience through healthy habits, you give your body its best chance to catch problems early or stop them before they start. Science continues to advance, but personal vigilance remains a cornerstone of long-term health.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?