It happens to many: you rise from a seated or lying position, and suddenly the room tilts. Your vision blurs, your head feels light, and for a few unsettling seconds, you wonder if you might collapse. This sensation—commonly dismissed as “standing up too fast”—is more than just a fleeting moment of imbalance. It’s often a sign of orthostatic hypotension, a condition where blood pressure drops significantly upon standing. While occasional dizziness may seem harmless, recurrent episodes can signal underlying health issues or increase fall risk, especially in older adults.
Understanding why this occurs—and how to manage it—is essential for maintaining daily function and long-term cardiovascular health. This article explores the physiology behind orthostatic hypotension, its triggers, who is most at risk, and what steps can be taken to reduce symptoms and improve stability.
What Is Orthostatic Hypotension?
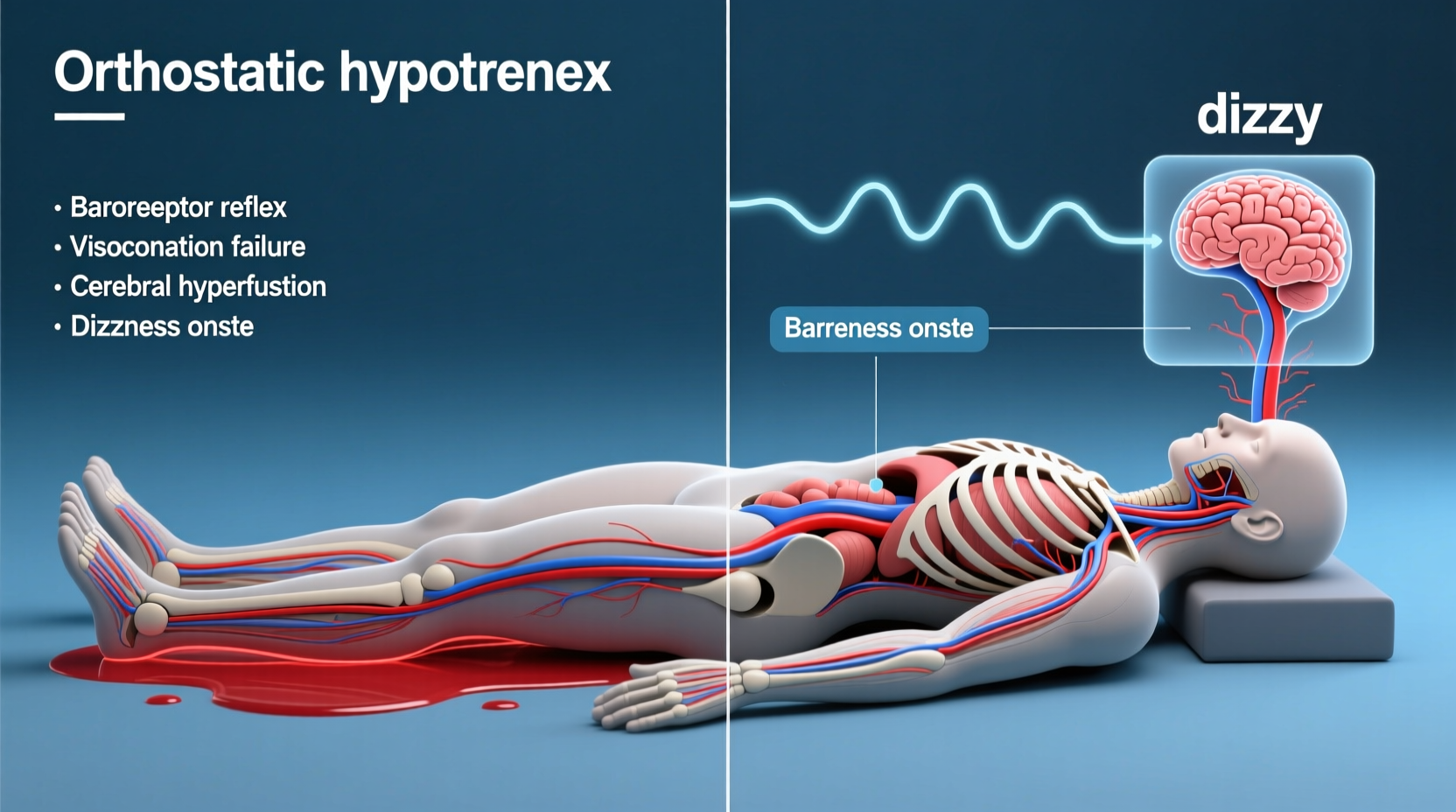
Orthostatic hypotension, also known as postural hypotension, is defined as a sudden drop in systolic blood pressure of at least 20 mm Hg or diastolic pressure of 10 mm Hg within three minutes of standing. This rapid decline impairs blood flow to the brain, leading to lightheadedness, blurred vision, weakness, or even fainting.
The human body relies on a finely tuned system to maintain consistent blood pressure across positions. When you lie down, blood distributes evenly throughout the body. Upon standing, gravity pulls blood downward into the legs and abdomen. To compensate, the autonomic nervous system signals the heart to beat faster and blood vessels to constrict, ensuring adequate perfusion to the brain.
In individuals with orthostatic hypotension, this regulatory mechanism falters. The response is either delayed, insufficient, or absent—resulting in transient cerebral hypoperfusion. The brain, deprived of oxygen-rich blood for even a few seconds, reacts with dizziness or disorientation.
Common Causes and Risk Factors
Orthostatic hypotension is not a disease in itself but rather a symptom of an underlying dysfunction. Several factors can impair the body’s ability to regulate blood pressure during positional changes.
Dehydration
Insufficient fluid intake reduces blood volume, making it harder for the circulatory system to maintain pressure. Even mild dehydration—such as after a night's sleep or during hot weather—can trigger symptoms.
Medications
Certain drugs are notorious for lowering blood pressure or interfering with autonomic control. These include:
- Diuretics (water pills)
- Alpha-blockers used for prostate issues
- Antidepressants, particularly tricyclics
- Anti-hypertensives for high blood pressure
- Parkinson’s disease medications
Aging and Autonomic Dysfunction
As people age, the baroreceptor reflex—the body’s natural blood pressure sensor—becomes less responsive. Additionally, conditions like diabetes can damage nerves involved in autonomic regulation, a disorder known as autonomic neuropathy.
Heart Conditions
Arrhythmias, heart valve problems, or heart failure can limit cardiac output, reducing the heart’s ability to compensate for posture changes.
Prolonged Bed Rest
Extended inactivity leads to deconditioning of the cardiovascular system. Astronauts returning from space and patients recovering from surgery often experience pronounced orthostatic intolerance due to reduced vascular tone.
“Orthostatic hypotension is more than a nuisance—it’s a red flag that should prompt evaluation, especially in older adults. Recurrent episodes correlate with increased risk of falls, stroke, and even dementia.” — Dr. Lena Patel, Neurocardiology Specialist, Johns Hopkins Medicine
Who Is Most at Risk?
While anyone can experience momentary dizziness when standing quickly, certain populations face higher susceptibility:
| Group | Risk Level | Primary Contributing Factors |
|---|---|---|
| Adults over 65 | High | Age-related nerve degeneration, polypharmacy, chronic illness |
| People with diabetes | High | Autonomic neuropathy, vascular stiffness |
| Individuals on antihypertensive drugs | Moderate to High | Excessive blood pressure reduction |
| Those with Parkinson’s disease | Very High | Neurodegeneration affecting autonomic control |
| Young adults with POTS | Moderate | Postural tachycardia syndrome (POTS), often misdiagnosed |
Interestingly, young, otherwise healthy individuals—particularly women—may also suffer from orthostatic intolerance. In such cases, conditions like postural orthostatic tachycardia syndrome (POTS) mimic orthostatic hypotension but are marked by a rapid heart rate increase instead of a significant blood pressure drop.
Recognizing Symptoms and Diagnosis
Symptoms typically begin within seconds to minutes of standing and resolve quickly when sitting or lying down. Common signs include:
- Dizziness or lightheadedness
- Blurred or tunnel vision
- Nausea
- Weakness or fatigue
- Fainting (syncope)
- Confusion or “brain fog”
To diagnose orthostatic hypotension, clinicians perform a simple test: measuring blood pressure and heart rate while the patient lies flat for 5 minutes, then immediately upon standing, and again at 1 and 3 minutes. A sustained drop confirms the diagnosis.
Further testing may include:
- Tilt-table testing to simulate positional changes in a controlled setting.
- Electrolyte panels to check for imbalances.
- Holter monitoring to assess heart rhythm.
- Autonomic function tests, including Valsalva maneuver and sudomotor testing.
Mini Case Study: Maria’s Morning Dizziness
Maria, a 72-year-old retired teacher, began experiencing frequent dizziness every morning when getting out of bed. Initially, she attributed it to aging. But after nearly falling while walking to the kitchen, she consulted her physician. Her blood pressure was normal while seated but dropped from 130/80 to 100/60 within two minutes of standing. Reviewing her medications revealed she was taking both a diuretic and an ACE inhibitor for hypertension—both contributing to excessive pressure reduction. Her doctor adjusted her dosage, advised gradual rising, and recommended increased salt and fluid intake. Within two weeks, her symptoms improved dramatically.
Managing and Preventing Episodes
For most people, orthostatic hypotension can be managed effectively through lifestyle modifications and medical oversight. The goal is to support blood pressure stability and enhance circulatory adaptation.
Step-by-Step Guide to Safer Position Changes
- Lie to Sit: Before getting out of bed, sit upright at the edge for 30–60 seconds.
- Ankle Pumps: While seated, flex and extend your ankles 10–15 times to promote venous return.
- Compression Maneuvers: Cross your legs or squeeze your thighs together briefly upon standing to help push blood upward.
- Pause and Breathe: Stand still for 10–15 seconds, focusing on steady breathing before walking.
- Hydrate First: Drink a glass of water upon waking; hydration improves blood volume and pressure regulation.
Hydration and Diet Adjustments
Maintaining adequate fluid intake is crucial. Aim for 1.5 to 2 liters of water daily unless contraindicated by heart or kidney disease. Some individuals benefit from slightly increasing dietary salt under medical supervision, as sodium helps retain fluid and boost blood pressure.
Large carbohydrate-heavy meals can worsen symptoms—a phenomenon called postprandial hypotension. Blood diverts to the digestive tract, leaving less available for the brain. Eating smaller, more frequent meals rich in protein and fiber can mitigate this effect.
Exercise and Physical Conditioning
Regular physical activity strengthens the cardiovascular system and improves autonomic responsiveness. Focus on low-impact exercises such as walking, swimming, or recumbent cycling. Avoid prolonged standing or exercising in hot environments, which can exacerbate symptoms.
Medication Review
Patients should have their medication list reviewed annually, especially if they’re on multiple drugs affecting blood pressure. Never discontinue prescribed medications without consulting a healthcare provider—but do raise concerns about dizziness as a side effect.
Checklist: Daily Habits to Reduce Dizziness
- ✅ Rise slowly from lying to sitting to standing
- ✅ Drink water first thing in the morning
- ✅ Avoid alcohol, which dilates blood vessels
- ✅ Wear compression stockings if recommended
- ✅ Eat balanced, small meals throughout the day
- ✅ Monitor blood pressure at home if possible
- ✅ Report frequent dizziness to your doctor
Frequently Asked Questions
Is it dangerous to feel dizzy when standing up?
Occasional dizziness after standing quickly is common and usually not serious. However, frequent or severe episodes—especially those accompanied by fainting, chest pain, or palpitations—should be evaluated. Persistent orthostatic hypotension increases the risk of falls, fractures, and cardiovascular events.
Can young people get orthostatic hypotension?
Yes. While more prevalent in older adults, younger individuals—particularly those with autoimmune disorders, eating disorders, or chronic fatigue—can develop orthostatic intolerance. In some cases, it’s linked to POTS or hypermobility syndromes like Ehlers-Danlos.
Does caffeine help with orthostatic hypotension?
Caffeine can cause a short-term increase in blood pressure and may offer temporary relief for some. However, its diuretic effect can contribute to dehydration, potentially worsening symptoms over time. Moderation is key.
Conclusion: Take Control of Your Stability
Dizziness upon standing is not something you must simply endure. Recognizing orthostatic hypotension as a legitimate physiological response—and not just a quirk of moving too fast—empowers you to take proactive steps toward better health. Whether it’s adjusting your morning routine, reviewing medications, or improving hydration and fitness, small changes can yield significant improvements in balance, energy, and safety.
If you or a loved one experiences regular lightheadedness when standing, don’t dismiss it. Speak with a healthcare provider, track your symptoms, and implement evidence-based strategies to support your body’s natural regulation. Your stability—and independence—depends on it.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?