You’ve probably experienced it: you stand up too fast from a seated or lying position and suddenly the room tilts, your vision blurs, and you feel lightheaded. This brief but disorienting sensation is more common than you might think. While often harmless, it can be a sign of an underlying condition known as postural hypotension—also called orthostatic hypotension. Understanding why this happens, what factors contribute to it, and how to manage it can help you maintain better balance, avoid falls, and improve daily comfort.
What Is Postural Hypotension?
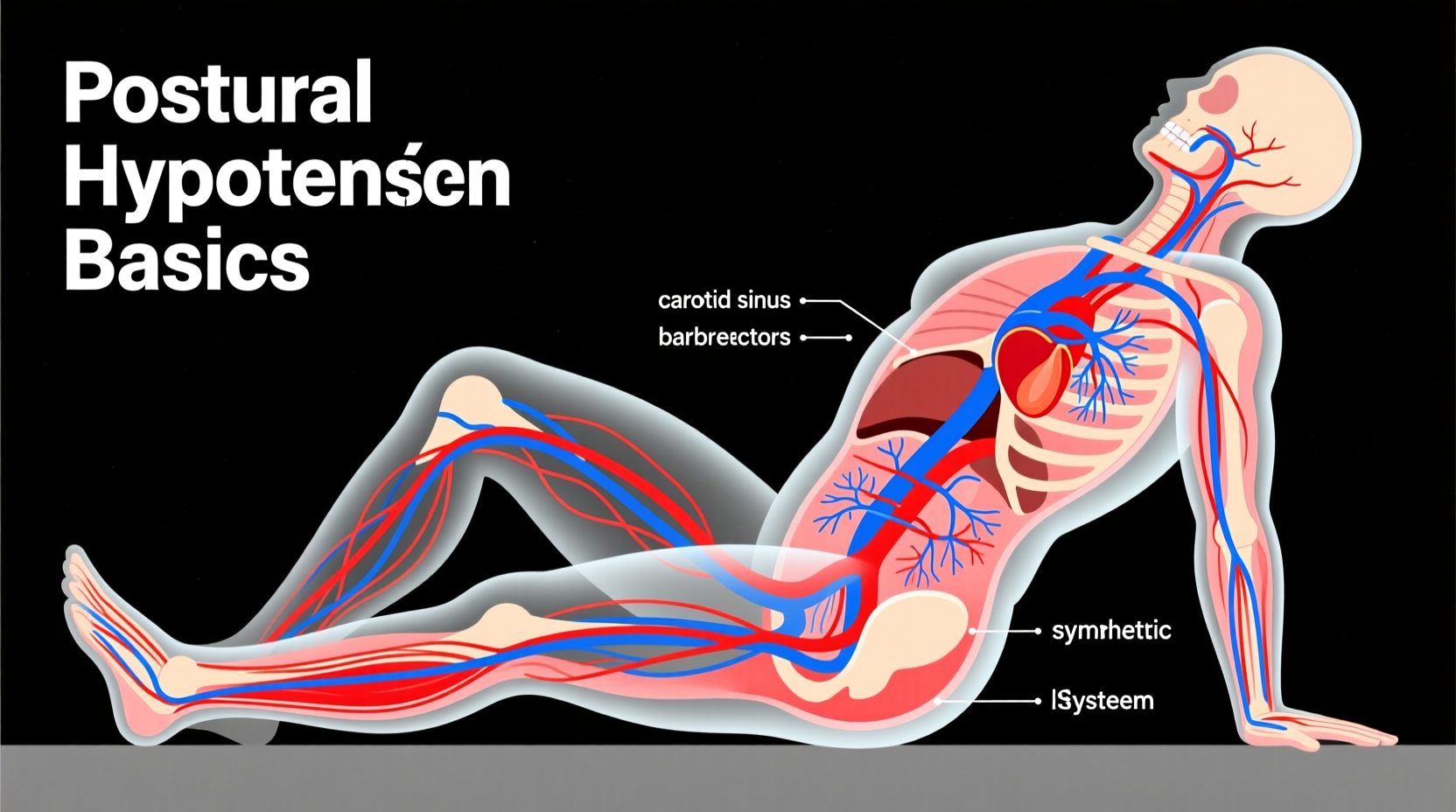
Postural hypotension occurs when your blood pressure drops significantly upon standing up from a sitting or lying position. Normally, when you change positions, your body automatically adjusts blood flow to ensure your brain receives a steady supply of oxygen-rich blood. This involves your autonomic nervous system constricting blood vessels and increasing heart rate to counteract gravity’s pull on blood pooling in your legs.
In postural hypotension, this compensatory mechanism fails or delays, leading to reduced blood flow to the brain for a few seconds. The result? Dizziness, lightheadedness, blurred vision, or even fainting.
The medical threshold for diagnosing orthostatic hypotension is a drop of at least 20 mm Hg in systolic blood pressure or 10 mm Hg in diastolic blood pressure within three minutes of standing.
“Orthostatic hypotension isn’t just about feeling dizzy—it’s a signal that the body’s circulatory regulation may need attention.” — Dr. Laura Simmons, Neurologist and Autonomic Specialist
Common Causes and Risk Factors
Several physiological and environmental factors can disrupt normal blood pressure regulation. Some are temporary; others point to chronic conditions. Knowing the root cause helps determine whether intervention is necessary.
Dehydration
Not drinking enough fluids reduces blood volume, making it harder for the body to maintain adequate pressure when upright. This is especially common in hot weather, after exercise, or during illness with vomiting or diarrhea.
Medications
Many prescription drugs lower blood pressure as part of their intended effect—or as a side effect. These include:
- Diuretics (water pills)
- Beta-blockers
- Alpha-blockers (used for prostate issues)
- Antidepressants (especially tricyclics)
- Parkinson’s disease medications
- Some erectile dysfunction drugs
Aging
As we age, our cardiovascular system becomes less responsive. Blood vessels lose elasticity, and the autonomic nervous system slows down, making older adults far more susceptible to postural drops in blood pressure.
Underlying Health Conditions
Certain disorders impair the body’s ability to regulate blood pressure effectively:
- Diabetes: Can damage nerves involved in blood pressure control (autonomic neuropathy).
- Parkinson’s disease: Affects autonomic function and often leads to orthostatic hypotension.
- Heart problems: Including arrhythmias, heart failure, or valve issues that limit cardiac output.
- Neurological disorders: Such as multiple system atrophy (MSA) or pure autonomic failure.
Extended Bed Rest
Spending long periods lying down weakens the body’s ability to adapt to upright posture. Astronauts returning from space and patients recovering from surgery often experience this type of transient hypotension.
Symptoms and When to Seek Help
The hallmark symptom of postural hypotension is dizziness upon standing, but it can present in several ways:
- Lightheadedness or feeling faint
- Blurred or tunnel vision
- Nausea
- Weakness
- Confusion or difficulty concentrating
- Fainting (syncope)
Episodes typically last only a few seconds to a minute and resolve once you sit or lie down. However, recurrent or severe symptoms—especially if they lead to falls—should not be ignored.
Seek medical evaluation if you experience:
- Frequent dizziness when standing
- Unexplained falls
- Chest pain or palpitations during episodes
- Shortness of breath
- Symptoms that interfere with daily activities
How Doctors Diagnose Orthostatic Hypotension
Diagnosis begins with a detailed history and physical exam. Your doctor will ask about your symptoms, medications, and any underlying health conditions. The key diagnostic test is the orthostatic vital signs measurement.
Step-by-Step Diagnostic Process
- You lie down for 5 minutes while your blood pressure and heart rate are recorded.
- You stand up slowly, and measurements are taken again at 1 and 3 minutes.
- A significant drop confirms orthostatic hypotension.
In more complex cases, additional tests may be used:
- Tilt table test: You’re strapped to a table that tilts from horizontal to vertical while vital signs are monitored.
- Autonomic function testing: Assesses how well your nervous system controls blood pressure and heart rate.
- Blood tests: To check for anemia, electrolyte imbalances, or endocrine disorders like adrenal insufficiency.
Effective Management and Prevention Strategies
Most cases of postural hypotension can be managed with lifestyle adjustments. For others, medication changes or targeted therapies may be needed.
Hydration and Salt Intake
Maintaining adequate fluid volume is crucial. Aim for 6–8 glasses of water per day unless restricted by a medical condition. In some cases, doctors recommend slightly increasing salt intake to help retain fluid and raise blood pressure—but only under supervision, especially for those with heart or kidney disease.
Compression Stockings
These tight-fitting garments apply pressure to the legs, reducing blood pooling and improving venous return to the heart. Waist-high compression stockings are most effective for orthostatic hypotension.
Physical Counterpressure Maneuvers
Simple techniques can prevent or reduce symptoms when you feel a spell coming on:
- Leg crossing while tensing thigh muscles
- Bending forward at the waist (like picking something up)
- Standing on tiptoes repeatedly
These actions squeeze blood back toward the heart and brain, helping stabilize blood pressure within seconds.
| Do | Don't |
|---|---|
| Rise slowly from sitting or lying positions | Stand up abruptly after prolonged rest |
| Stay hydrated throughout the day | Go long periods without drinking fluids |
| Perform counterpressure maneuvers when dizzy | Ignore warning signs and try to \"push through\" dizziness |
| Review medications with your doctor regularly | Assume all dizziness is normal aging |
Medication Adjustments
If a drug is contributing to low blood pressure, your doctor may reduce the dose, switch medications, or change the timing. Never stop or alter prescribed medication without professional guidance.
In persistent cases, specific medications may be prescribed to increase blood volume or constrict blood vessels, such as:
- Fludrocortisone (promotes sodium retention)
- Midodrine (a vasoconstrictor)
- Droxidopa (used in neurogenic orthostatic hypotension)
Real-Life Example: Managing Symptoms After Surgery
John, a 72-year-old recovering from hip replacement surgery, spent nearly two weeks mostly in bed. When he attempted to stand for the first time with assistance, he immediately felt his vision darken and had to sit back down. Nurses suspected orthostatic hypotension due to deconditioning and fluid shifts.
His care team implemented a gradual mobilization plan: starting with sitting on the edge of the bed for 1–2 minutes, then progressing to standing with support. He was encouraged to drink extra fluids and wear compression stockings. Within days, his tolerance improved significantly, and he could walk short distances without dizziness.
This case highlights how temporary factors—like immobility and anesthesia aftereffects—can trigger postural hypotension, but structured interventions make a meaningful difference.
Checklist: Daily Habits to Reduce Dizziness
Use this checklist to minimize episodes of lightheadedness when standing:
- ✅ Drink water consistently throughout the day
- ✅ Rise slowly: sit up first, pause, then stand
- ✅ Avoid prolonged standing, especially in hot environments
- ✅ Wear compression stockings if recommended
- ✅ Review all medications with your physician annually
- ✅ Perform leg exercises before standing (e.g., ankle pumps)
- ✅ Eat balanced meals and avoid alcohol, which can worsen symptoms
Frequently Asked Questions
Is dizziness when standing up a sign of low iron?
Yes, anemia (often caused by iron deficiency) can contribute to dizziness upon standing. Low red blood cell count reduces oxygen delivery to the brain, amplifying symptoms of poor circulation. Blood tests can confirm whether anemia is a factor.
Can anxiety cause similar symptoms?
Anxiety can mimic dizziness and lightheadedness, but it usually occurs regardless of posture and is accompanied by other symptoms like rapid breathing, sweating, or a racing heart. True orthostatic hypotension is directly tied to positional change and resolves quickly with sitting or lying down.
Should I worry if this only happens occasionally?
Occasional mild dizziness when rising quickly is common and usually not dangerous. However, if it becomes frequent, severe, or starts affecting your balance or safety, it's worth discussing with a healthcare provider.
Conclusion: Listen to Your Body and Take Action
Feeling dizzy when standing up quickly is more than just a minor inconvenience—it’s your body signaling that something in its regulatory system needs attention. While many cases stem from benign, fixable causes like dehydration or quick movements, recurring symptoms deserve proper evaluation. With smart habits, medical awareness, and timely intervention, postural hypotension can be managed effectively.
Start by slowing your transitions, staying hydrated, and monitoring your symptoms. Share concerns with your doctor, especially if dizziness interferes with independence or safety. Small changes today can prevent bigger complications tomorrow.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?