Facial twitching—those sudden, involuntary contractions of muscles around the eye, cheek, or mouth—is something most people experience at least once. While usually harmless, persistent or frequent twitching can be unsettling. Many assume it’s just fatigue or stress, but the truth is more complex. Behind seemingly random facial twitches are a range of physiological, neurological, and lifestyle-driven factors—some of which may surprise you.
This article explores the science behind facial twitching, identifies common and lesser-known triggers, and offers practical steps to manage and reduce episodes. Understanding what’s really causing your face to twitch is the first step toward regaining control—and peace of mind.
The Science Behind Facial Twitching
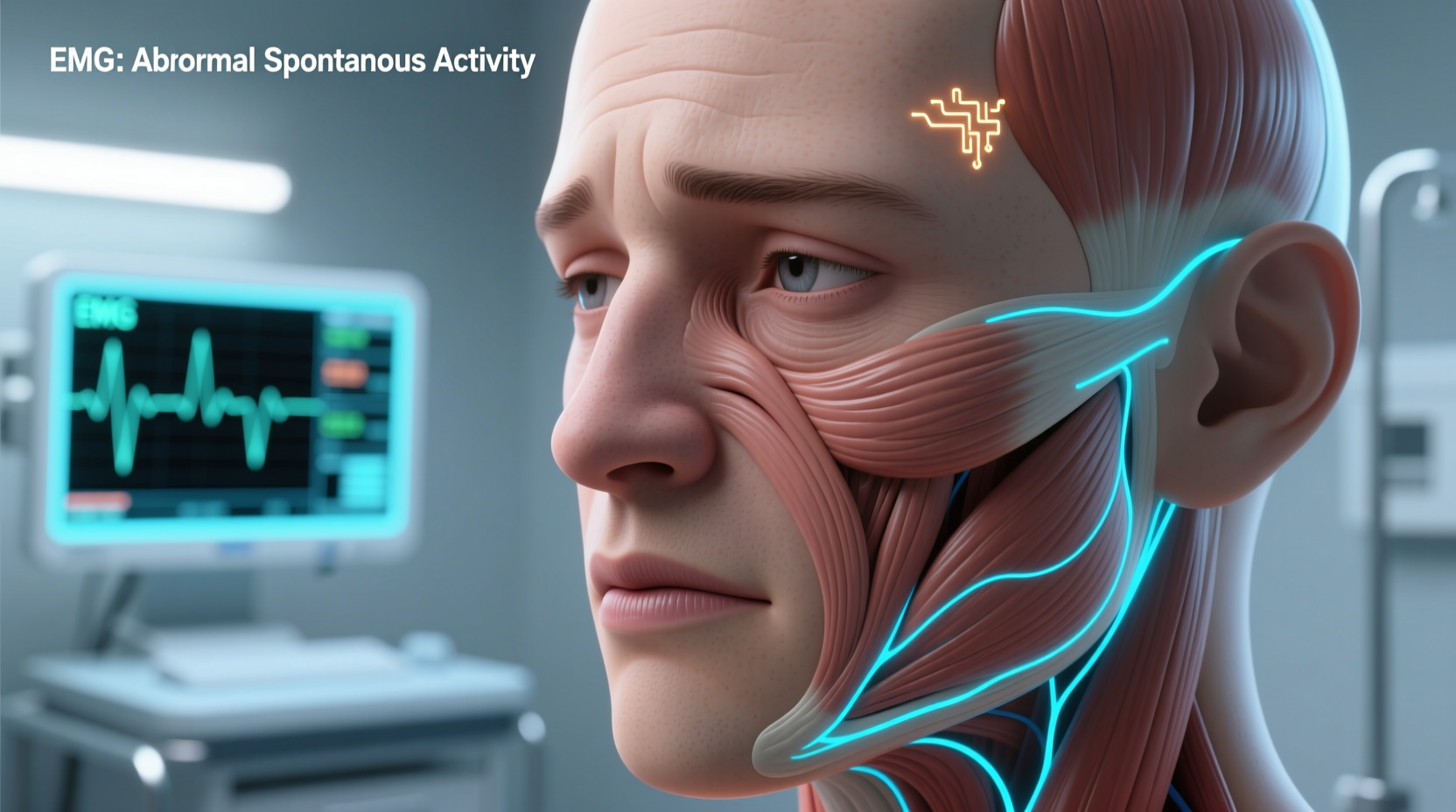
Facial twitches, medically known as fasciculations, occur when small groups of muscle fibers contract involuntarily. These contractions are typically caused by misfiring signals from the nerves that control the muscles. In most cases, they’re benign and temporary, affecting areas like the eyelid (commonly called \"eye jumping\"), corner of the mouth, or lower cheek.
The facial nerve (cranial nerve VII) controls the muscles of facial expression. When this nerve becomes irritated or overstimulated—due to internal imbalances or external pressures—it can send erratic signals, leading to twitching. While occasional twitching is normal, chronic or spreading spasms may indicate underlying conditions such as:
- Bell’s palsy: A condition causing temporary facial paralysis due to inflammation of the facial nerve.
- Hemifacial spasm: Persistent unilateral twitching often linked to blood vessel compression on the nerve.
- Neurological disorders: Rarely, conditions like multiple sclerosis or Parkinson’s disease may present with facial twitching early on.
For the vast majority, however, no serious pathology is involved. Instead, the culprits lie in everyday habits and overlooked lifestyle factors.
Common Triggers You Already Know
Some causes of facial twitching are well-documented and widely recognized:
- Stress and Anxiety: High cortisol levels disrupt nerve function and increase muscle tension, making twitching more likely.
- Sleep Deprivation: Poor sleep impairs nervous system regulation, increasing the likelihood of neuromuscular misfires.
- Caffeine Overload: Stimulants heighten nerve excitability. Excess coffee, energy drinks, or even dark chocolate can trigger spasms.
- Dry Eyes or Eye Strain: Especially for eyelid twitching, prolonged screen use or uncorrected vision issues contribute significantly.
These are valid starting points—but they don’t tell the whole story. What many people overlook are the subtle, cumulative triggers that fly under the radar.
Surprising Triggers That Might Be Causing Your Twitch
Beyond the usual suspects, several lesser-known factors can provoke facial twitching. These often go unnoticed because their effects are delayed or indirect.
Nutrient Deficiencies
Electrolytes and minerals play a critical role in nerve signaling and muscle contraction. Deficiencies in magnesium, potassium, calcium, or vitamin B12 can lead to hyperexcitable nerves and muscle spasms.
Magnesium, in particular, acts as a natural calcium blocker and helps regulate neurotransmitters. Low levels—common in diets high in processed foods or due to chronic stress—can manifest as eyelid or cheek twitching.
“Magnesium deficiency is one of the most underdiagnosed nutritional issues contributing to neuromuscular irritability—including facial twitching.” — Dr. Lena Patel, Neurologist and Nutritional Medicine Specialist
Screen Blue Light Exposure
Extended exposure to blue light from smartphones, laptops, and LED screens doesn’t just strain your eyes—it disrupts circadian rhythms and increases oxidative stress in neural tissues. This imbalance can heighten nerve sensitivity, especially in individuals already prone to twitching.
A 2023 study published in *Neurological Sciences* found that participants who spent over 9 hours daily on digital devices were 2.3 times more likely to report chronic eyelid twitching than those with less than 5 hours of screen time.
Dehydration
Even mild dehydration alters electrolyte balance and reduces blood flow to nerves. When brain cells and peripheral nerves don’t receive optimal hydration, they become more prone to erratic firing. A person might not feel thirsty yet still be dehydrated enough to trigger muscle fasciculations.
Sodium Imbalance
Both too much and too little sodium can cause problems. High sodium leads to fluid retention and nerve swelling; low sodium (hyponatremia), often seen in endurance athletes or those on aggressive water-drinking regimens, disrupts electrical signaling. Either extreme may result in twitching.
Medication Side Effects
Certain medications list muscle twitching as a rare side effect. These include:
- Antipsychotics (e.g., haloperidol)
- Antihistamines (especially first-generation types like diphenhydramine)
- Stimulant ADHD medications (e.g., Adderall)
- Some asthma inhalers containing beta-agonists
If you started a new medication around the time twitching began, consult your doctor before making changes.
Posture and Neck Tension
Poor posture—especially forward head positioning while working at a desk—compresses nerves in the cervical spine. The greater auricular nerve and other branches feeding into the facial region can become irritated, indirectly influencing facial muscle activity.
What You Can Do: Practical Steps to Reduce Twitching
Most facial twitching resolves on its own, but proactive management can shorten duration and prevent recurrence. Here’s a step-by-step guide based on clinical recommendations and patient outcomes.
Step-by-Step Guide to Managing Facial Twitching
- Assess Your Lifestyle Habits: Log your daily routine for one week. Note caffeine intake, sleep duration, screen time, and stress levels. Look for correlations with twitching episodes.
- Hydrate Strategically: Aim for 2–2.5 liters of water daily, but pair it with electrolyte sources like bananas, spinach, avocado, or a pinch of sea salt in water. Avoid chugging large amounts at once.
- Reduce Caffeine Gradually: Cut back by 25% every 3–4 days to avoid withdrawal headaches. Replace coffee with herbal teas like chamomile or rooibos.
- Optimize Sleep Hygiene: Maintain a consistent bedtime, avoid screens 60–90 minutes before bed, and keep your bedroom cool and dark.
- Incorporate Magnesium-Rich Foods: Add pumpkin seeds, almonds, black beans, and dark leafy greens to your diet. Consider a supplement (200–400 mg/day of magnesium glycinate) after consulting your physician.
- Use Blue Light Filters: Enable night mode on devices or wear blue-blocking glasses in the evening. Limit recreational screen use after 8 PM.
- Practice Gentle Neck Stretches: Perform slow neck rolls and lateral stretches twice daily to relieve cervical tension.
- Apply Warm Compresses: For eyelid twitching, a warm cloth applied for 5 minutes twice a day can relax the orbicularis oculi muscle.
Checklist: Daily Actions to Prevent Facial Twitching
- ✅ Drink at least 8 glasses of water with balanced electrolytes
- ✅ Limit caffeine to under 200 mg (about one strong coffee)
- ✅ Get 7–8 hours of uninterrupted sleep
- ✅ Take a 5-minute screen break every hour
- ✅ Eat one magnesium-rich food (e.g., spinach, nuts, whole grains)
- ✅ Perform 3 minutes of neck and shoulder stretches
- ✅ Use artificial tears if eyes feel dry (preservative-free preferred)
- ✅ Practice deep breathing or mindfulness for 5 minutes
When to See a Doctor
While most facial twitching is benign, certain red flags warrant medical evaluation:
| Symptom | Benign Twitching | Seek Medical Advice |
|---|---|---|
| Duration | Seconds to minutes; resolves in days | Persistent for weeks or worsening |
| Location | One small area (e.g., eyelid) | Spreading to other facial zones |
| Associated Symptoms | None or mild eye dryness | Drooping eyelid, facial weakness, pain |
| Triggers | Stress, caffeine, fatigue | Occurs at rest, unrelated to habits |
If twitching spreads, becomes constant, or is accompanied by facial droop, difficulty closing the eye, or pain, see a neurologist. Hemifacial spasm or nerve compression may require imaging (like an MRI) or treatments such as Botox injections or microvascular decompression surgery.
Real-Life Example: Sarah’s Story
Sarah, a 34-year-old graphic designer, began experiencing left eyelid twitching that lasted over three weeks. She assumed it was stress-related due to a tight project deadline. Despite cutting coffee and trying eye drops, the twitch persisted.
After tracking her habits, she noticed she was drinking 3 liters of water daily but eating very few salty or mineral-rich foods. Blood tests revealed low magnesium and slightly low sodium levels. Her doctor advised reducing water intake slightly and adding magnesium supplements and electrolyte-rich meals.
Within 10 days, the twitching stopped. “I never thought drinking too much water could be the problem,” Sarah said. “Now I balance hydration with nutrition—and my face hasn’t twitched since.”
Frequently Asked Questions
Can anxiety really cause facial twitching?
Yes. Anxiety increases adrenaline and cortisol, which heighten nerve sensitivity and muscle tension. This combination can trigger or worsen facial twitching, particularly around the eyes and jaw. Managing stress through therapy, breathing exercises, or meditation often reduces symptoms.
Is facial twitching a sign of a stroke?
Isolated, brief facial twitching is not a sign of stroke. However, if twitching is accompanied by facial drooping, slurred speech, arm weakness, or confusion, seek emergency care immediately. These could indicate a transient ischemic attack (TIA) or stroke.
Can lack of sleep cause long-term twitching?
Chronic sleep deprivation can lead to sustained neuromuscular irritation, prolonging twitching episodes. Over time, poor sleep disrupts the autonomic nervous system, increasing the risk of recurrent fasciculations. Prioritizing consistent, quality sleep is essential for resolution.
Take Control of Your Nervous System
Your face twitching isn’t random—it’s a signal. Whether it's your body asking for more rest, better hydration, or reduced screen exposure, listening closely can prevent minor spasms from becoming chronic issues. The triggers may surprise you, but the solutions are within reach.
Start today: adjust your habits, track your progress, and give your nervous system the support it needs. Most people see improvement within days of making simple, sustainable changes. If symptoms persist, don’t hesitate to consult a healthcare provider—early intervention ensures peace of mind and optimal outcomes.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?