Bloating after meals is one of the most common digestive complaints—yet it’s often dismissed as normal. While occasional bloating may not be cause for concern, frequent or severe post-meal distension can interfere with daily life and indicate underlying imbalances in digestion. The good news: most causes are manageable through dietary and lifestyle adjustments. Understanding what triggers bloating and how to respond effectively can transform your comfort and confidence at every meal.
What Causes Post-Meal Bloating?
Bloating refers to the sensation of fullness, tightness, or swelling in the abdomen, often accompanied by gas, rumbling, or visible distension. It typically occurs when gas builds up in the digestive tract or when food moves too slowly through the intestines. While some degree of gas production is natural, persistent bloating suggests that something in your diet or gut function needs attention.
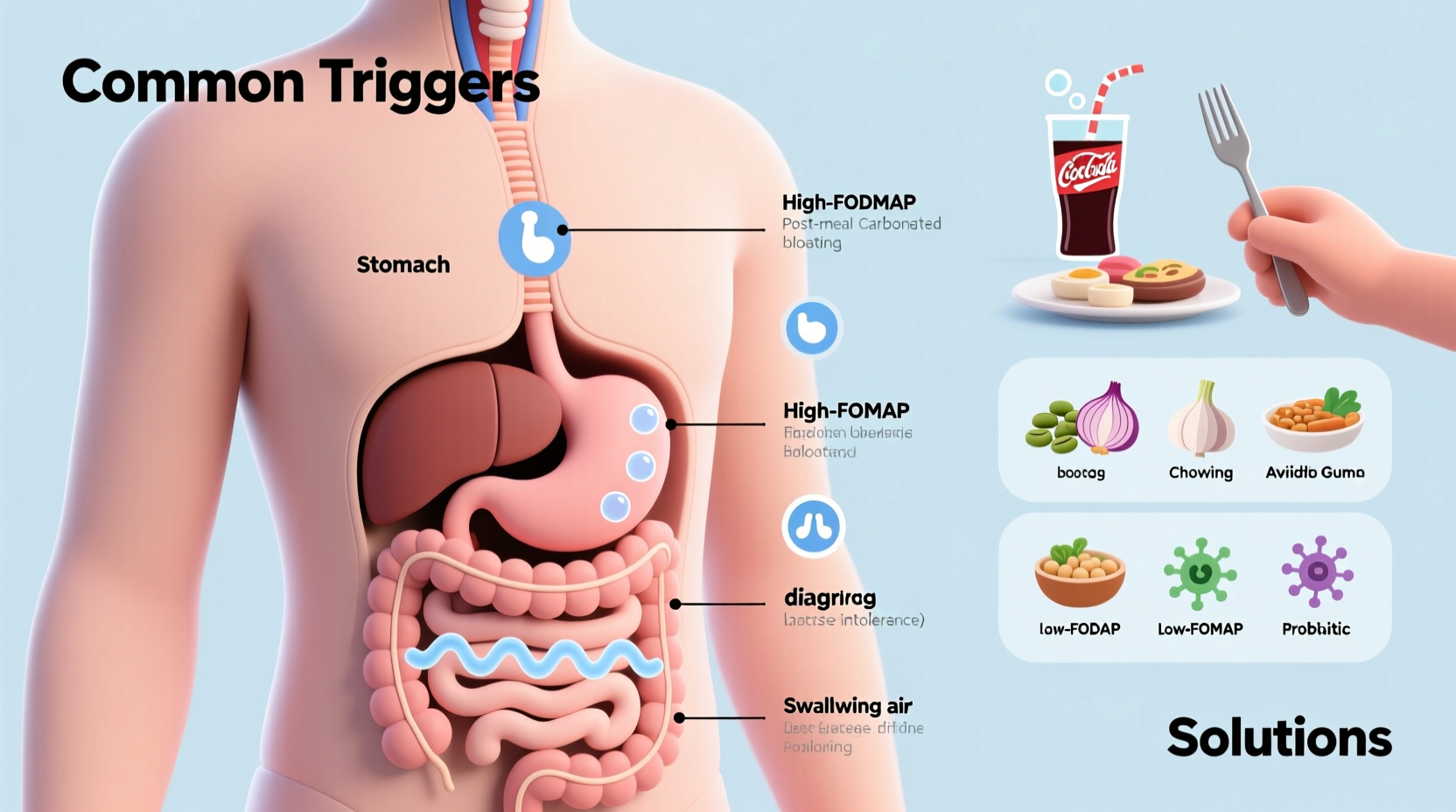
The digestive system breaks down food using enzymes, acids, and gut bacteria. When this process is disrupted—by eating habits, food sensitivities, or gut microbiome imbalance—it can lead to fermentation, excess gas, and inflammation. Common contributors include:
- Dietary choices: High-FODMAP foods, carbonated drinks, artificial sweeteners.
- Eating behaviors: Eating too quickly, overeating, or swallowing air (aerophagia).
- Food intolerances: Lactose, fructose, gluten, or histamine intolerance.
- Gut motility issues: Slow transit time due to IBS, constipation, or stress.
- Microbiome imbalance: Overgrowth of certain bacteria (like SIBO) or yeast.
“Bloating is a symptom, not a diagnosis. Identifying the root cause is essential for long-term relief.” — Dr. Lena Torres, Gastroenterology Specialist
Common Dietary Triggers and How to Spot Them
Foods play a central role in post-meal bloating. Some ingredients ferment easily in the colon, producing hydrogen, methane, or carbon dioxide. Others draw water into the intestines or trigger immune responses in sensitive individuals.
High-FODMAP Foods
FODMAP stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols—short-chain carbohydrates poorly absorbed in the small intestine. When they reach the colon, gut bacteria ferment them, releasing gas.
Common high-FODMAP foods include:
- Onions, garlic, leeks
- Apples, pears, mangoes
- Wheat, rye, barley
- Milk, yogurt, soft cheeses
- Legumes like beans and lentils
- Sugar alcohols (xylitol, sorbitol) in sugar-free gum
Lactose and Dairy Sensitivity
Lactose, the sugar in milk, requires the enzyme lactase for digestion. Many adults produce less lactase with age, leading to undigested lactose fermenting in the colon. Symptoms include bloating, cramping, and diarrhea within 30 minutes to two hours after consuming dairy.
Carbonated Beverages and Artificial Sweeteners
Soda, sparkling water, and diet drinks introduce excess air and fermentable compounds into the gut. Artificial sweeteners like sucralose and aspartame may disrupt gut bacteria, while sugar alcohols (common in “sugar-free” products) are notorious for causing gas and bloating.
Processed and High-Sodium Foods
Packaged meals, canned soups, and fast food are loaded with sodium, which causes water retention. This leads to temporary abdominal puffiness—even without gas buildup.
Step-by-Step Guide to Reducing Bloating
Eliminating bloating isn’t about cutting out entire food groups permanently—it’s about identifying patterns and making sustainable changes. Follow this practical sequence to pinpoint and address your triggers.
- Keep a food and symptom journal for 7–10 days. Record everything you eat, drink, and any bloating symptoms (timing, severity, associated factors like stress).
- Reduce obvious irritants: Eliminate carbonated drinks, chewing gum, and processed foods high in sodium and additives.
- Try a low-FODMAP trial for 3–4 weeks under guidance. Reintroduce foods systematically to test tolerance.
- Modify eating habits: Eat slowly, chew thoroughly, and avoid large portions.
- Test for food intolerances via breath tests (for lactose, fructose, SIBO) or elimination diets.
- Support digestion: Consider digestive enzymes (like lactase or alpha-galactosidase for beans) if needed.
- Reassess gut health with a healthcare provider if symptoms persist.
Bloating Triggers vs. Fixes: Quick Reference Table
| Trigger | Why It Causes Bloating | Effective Fix |
|---|---|---|
| Onions & Garlic | High in fructans (FODMAPs), fermented by gut bacteria | Use garlic-infused oil instead; limit raw intake |
| Carbonated Drinks | Introduce excess CO₂ into the digestive tract | Switch to still water, herbal teas, or diluted juices |
| Chewing Gum | Causes air swallowing and contains sugar alcohols | Avoid gum; try fennel seeds or peppermint tea post-meal |
| Large Meals | Overwhelm digestive capacity, slow gastric emptying | Eat smaller, more frequent meals; stop before feeling full |
| Lactose-Rich Foods | Undigested lactose ferments in colon | Choose lactose-free dairy or take lactase enzyme supplements |
Real-Life Example: Sarah’s Journey to Relief
Sarah, a 34-year-old teacher, experienced daily bloating after lunch, often so severe she avoided social events. She assumed it was “just how her body worked.” After tracking her meals, she noticed bloating consistently followed salads with onions, apples, and goat cheese—three high-FODMAP foods. She also drank two cans of sparkling water daily.
With the help of a dietitian, Sarah eliminated high-FODMAP foods and carbonation for three weeks. Her bloating reduced by 80%. During reintroduction, she discovered she could tolerate small amounts of apple but not onions or goat cheese. By swapping ingredients and drinking still water with lemon, she now enjoys meals without discomfort.
Expert-Backed Tips to Prevent Bloating
Small habit changes can yield significant results. These strategies are supported by clinical research and digestive health professionals.
Incorporate these habits gradually. Consistency matters more than perfection.
When to See a Doctor
While most bloating is benign, certain red flags warrant medical evaluation:
- Unintentional weight loss
- Blood in stool
- Persistent diarrhea or constipation
- Nighttime symptoms disrupting sleep
- Family history of celiac disease, IBD, or colon cancer
Conditions like irritable bowel syndrome (IBS), small intestinal bacterial overgrowth (SIBO), celiac disease, or inflammatory bowel disease (IBD) can present with chronic bloating. Diagnostic tools such as hydrogen breath tests, blood panels, or endoscopies may be necessary.
Bloating Prevention Checklist
Use this checklist daily to minimize bloating risk:
- ✅ Eat slowly and chew food thoroughly
- ✅ Avoid carbonated beverages and chewing gum
- ✅ Limit high-FODMAP foods if sensitive
- ✅ Choose lactose-free options if dairy causes issues
- ✅ Stay hydrated with non-carbonated fluids
- ✅ Take a 10-minute walk after meals
- ✅ Manage stress through breathing, meditation, or yoga
- ✅ Keep a food-symptom journal weekly
Frequently Asked Questions
Is bloating the same as weight gain?
No. Bloating is temporary swelling caused by gas, fluid, or slow digestion. It fluctuates throughout the day and resolves with burping, passing gas, or bowel movements. Weight gain involves increased body fat and is measured over time, not hour-to-hour.
Can stress really cause bloating?
Yes. The gut and brain are closely linked through the gut-brain axis. Stress activates the sympathetic nervous system, slowing digestion and altering gut motility. This can lead to food stagnating in the intestines, increasing fermentation and gas production. Chronic stress may also worsen IBS symptoms.
Are probiotics helpful for bloating?
It depends on the individual and strain. Some people find relief with specific probiotics like Bifidobacterium infantis or Lactobacillus acidophilus, especially in IBS. However, others may feel worse initially as the microbiome adjusts. Start with a low dose and choose evidence-based strains. Consult a professional if unsure.
Conclusion: Take Control of Your Digestive Comfort
Bloating after meals doesn’t have to be a routine part of your life. With careful observation and targeted changes, most people can significantly reduce or eliminate discomfort. Start by tuning into your body’s signals, adjusting your eating habits, and eliminating common triggers. Remember, digestion is deeply personal—what works for one person may not work for another. Patience and persistence are key.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?