Suddenly standing from a seated or lying position and experiencing blurred vision is more common than many realize. Often dismissed as a fleeting inconvenience, this phenomenon can signal underlying physiological shifts—some benign, others worth monitoring. While occasional lightheadedness or visual disturbance may not be cause for alarm, frequent or severe episodes could point to cardiovascular, neurological, or metabolic concerns. Understanding the mechanisms behind this response helps distinguish normal bodily reactions from warning signs that require attention.
The Science Behind Blurred Vision Upon Standing
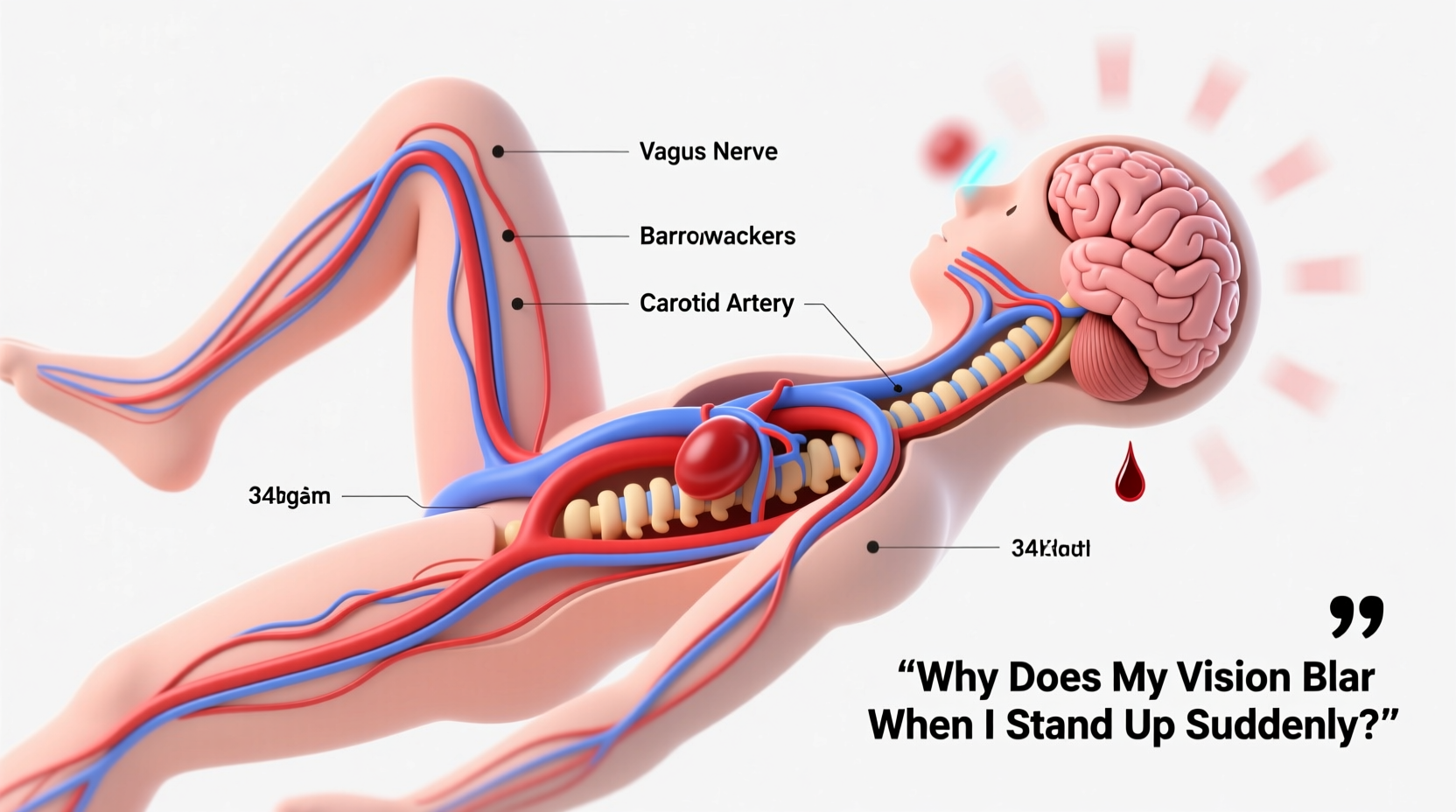
When you transition rapidly from sitting or lying down to standing, gravity pulls blood downward into the lower extremities. This temporary pooling reduces the volume of blood returning to the heart and brain, leading to a brief drop in blood pressure—a condition known as orthostatic hypotension. The brain, particularly the visual cortex and ocular blood supply, is highly sensitive to even minor reductions in oxygen delivery. As cerebral perfusion dips momentarily, visual processing can falter, resulting in blurred vision, tunnel vision, or even temporary graying out of sight.
This process typically resolves within seconds as the body’s autonomic nervous system compensates: blood vessels constrict, heart rate increases, and circulation stabilizes. However, if these regulatory mechanisms lag or are impaired, symptoms may persist longer or intensify.
Common Causes and Contributing Factors
While orthostatic hypotension is the primary explanation, several factors influence its frequency and severity:
- Dehydration: Low fluid volume reduces overall blood pressure, making it harder for the body to maintain cerebral flow during positional changes.
- Medications: Diuretics, antihypertensives, antidepressants, and Parkinson’s drugs can interfere with vascular tone or heart rate regulation.
- Age-related changes: Baroreceptor sensitivity declines with age, slowing the body’s ability to adjust blood pressure quickly.
- Prolonged bed rest: Inactivity weakens circulatory responsiveness, increasing susceptibility upon reambulation.
- Dietary habits: Skipping meals or consuming large carbohydrate-heavy meals can trigger postprandial hypotension, exacerbating dizziness after eating.
In younger individuals, especially tall adolescents or those with a lean build, a heightened vagal response can also contribute. Known as vasovagal syncope, this reflex causes a sudden drop in heart rate and blood pressure, often preceded by visual disturbances, nausea, or sweating.
When It Might Signal an Underlying Condition
Occasional mild blurring upon standing is usually harmless. However, recurrent or disabling symptoms may indicate conditions requiring medical evaluation:
- Autonomic Dysfunction: Disorders like postural orthostatic tachycardia syndrome (POTS) or pure autonomic failure impair the nervous system’s control over blood pressure and heart rate.
- Anemia: Reduced red blood cell count limits oxygen-carrying capacity, amplifying symptoms of low perfusion.
- Cardiac issues: Arrhythmias, valve disorders, or heart failure can compromise cardiac output during postural shifts.
- Neurological diseases: Multiple sclerosis, Parkinson’s disease, or diabetic neuropathy may damage autonomic nerves involved in blood pressure regulation.
- Endocrine imbalances: Adrenal insufficiency (e.g., Addison’s disease) affects electrolyte balance and vascular tone.
“Recurrent presyncope or visual blurring upon standing should never be ignored, especially in older adults. It's a window into cardiovascular resilience.” — Dr. Lena Torres, Neurologist and Autonomic Specialist, Mayo Clinic
Step-by-Step Guide to Managing and Preventing Episodes
If you experience blurred vision when standing, consider implementing the following steps to reduce frequency and severity:
- Hydrate consistently: Aim for at least 1.5–2 liters of water daily, more in hot climates or during physical activity. Adding a pinch of salt to fluids (if medically safe) can help retain volume.
- Rise gradually: After waking or sitting, spend 30 seconds with your legs dangling off the bed or chair. Flex your calf muscles before standing to pump blood upward.
- Monitor medication effects: Review prescriptions with your doctor. Some medications can be adjusted in timing or dosage to minimize orthostatic effects.
- Wear compression stockings: These help prevent blood from pooling in the legs, supporting venous return.
- Stay physically active: Regular aerobic exercise improves vascular tone and autonomic responsiveness. Focus on walking, cycling, or swimming.
- Avoid triggers: Limit alcohol, large meals, and prolonged standing in hot environments—all of which can worsen blood pressure drops.
Mini Case Study: Sarah’s Experience with POTS
Sarah, a 24-year-old graduate student, began noticing frequent episodes of blurred vision and near-fainting when standing between lectures. Initially attributing it to stress and caffeine intake, she found symptoms worsening over months. After collapsing during a lab session, she sought medical evaluation. Tilt-table testing confirmed postural orthostatic tachycardia syndrome (POTS), characterized by a heart rate increase of over 30 bpm upon standing without significant blood pressure drop. With guidance from her care team, Sarah adopted increased fluid and salt intake, wore compression garments, and incorporated strength training. Within three months, her symptoms improved dramatically, allowing her to resume full academic and social activities.
Do’s and Don’ts: Quick Reference Table
| Do | Don’t |
|---|---|
| Drink water throughout the day | Go long periods without hydrating |
| Stand up slowly after resting | Jump up quickly from bed or couch |
| Perform leg muscle contractions before rising | Stand still immediately after getting up |
| Track symptoms in a journal | Ignore recurring dizziness or vision changes |
| Consult a doctor if symptoms worsen | Self-diagnose or stop medications abruptly |
FAQ: Common Questions About Vision Blurring When Standing
Is it normal to see black spots or blur when standing up?
Yes, seeing brief darkening, blurring, or “floaters” when standing quickly is common and often due to transient cerebral hypoperfusion. If episodes last more than a few seconds, occur frequently, or are accompanied by chest pain, palpitations, or confusion, consult a healthcare provider.
Can low iron cause blurred vision upon standing?
Indirectly, yes. Iron deficiency anemia reduces oxygen delivery to tissues, including the brain. This lowers the threshold for symptoms during blood pressure fluctuations, making dizziness and visual disturbances more likely when changing positions.
Should I worry if only one episode happened?
A single, isolated incident—especially after dehydration, illness, or skipping meals—is usually not concerning. However, if it recurs or progresses in intensity, further assessment is warranted to rule out chronic conditions.
Checklist: What to Do If You Frequently Experience Blurry Vision When Standing
- ✅ Assess hydration: Are you drinking enough water daily?
- ✅ Review medications: Are any known to affect blood pressure?
- ✅ Monitor symptoms: Keep a log of frequency, duration, and triggers.
- ✅ Check for additional signs: Note fatigue, rapid heartbeat, or fainting.
- ✅ Schedule a check-up: Include blood pressure readings both lying and standing.
- ✅ Consider blood tests: CBC, electrolytes, glucose, and thyroid function.
- ✅ Try preventive strategies: Compression wear, slow rising, increased salt (if approved).
Conclusion: Listen to Your Body’s Signals
Blurred vision upon standing is often a minor physiological hiccup, but it can also serve as an early alert system for deeper health dynamics. By paying attention to patterns, adjusting lifestyle habits, and seeking timely medical input when needed, you can safeguard both short-term comfort and long-term well-being. Don’t dismiss repeated symptoms as mere fatigue or aging—they may be guiding you toward better self-care and earlier intervention.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?