Suddenly standing from a seated or lying position and experiencing blurred vision, dizziness, or even momentary blackouts is more common than many realize. While often harmless, this phenomenon can sometimes signal underlying health issues that require attention. Known medically as orthostatic hypotension—or postural hypotension—it occurs when blood pressure drops rapidly upon standing, reducing blood flow to the brain and affecting visual clarity. Understanding the mechanics behind this response, recognizing contributing factors, and knowing when to consult a healthcare provider are essential steps in maintaining long-term cardiovascular and neurological health.
The Science Behind Blurred Vision Upon Standing
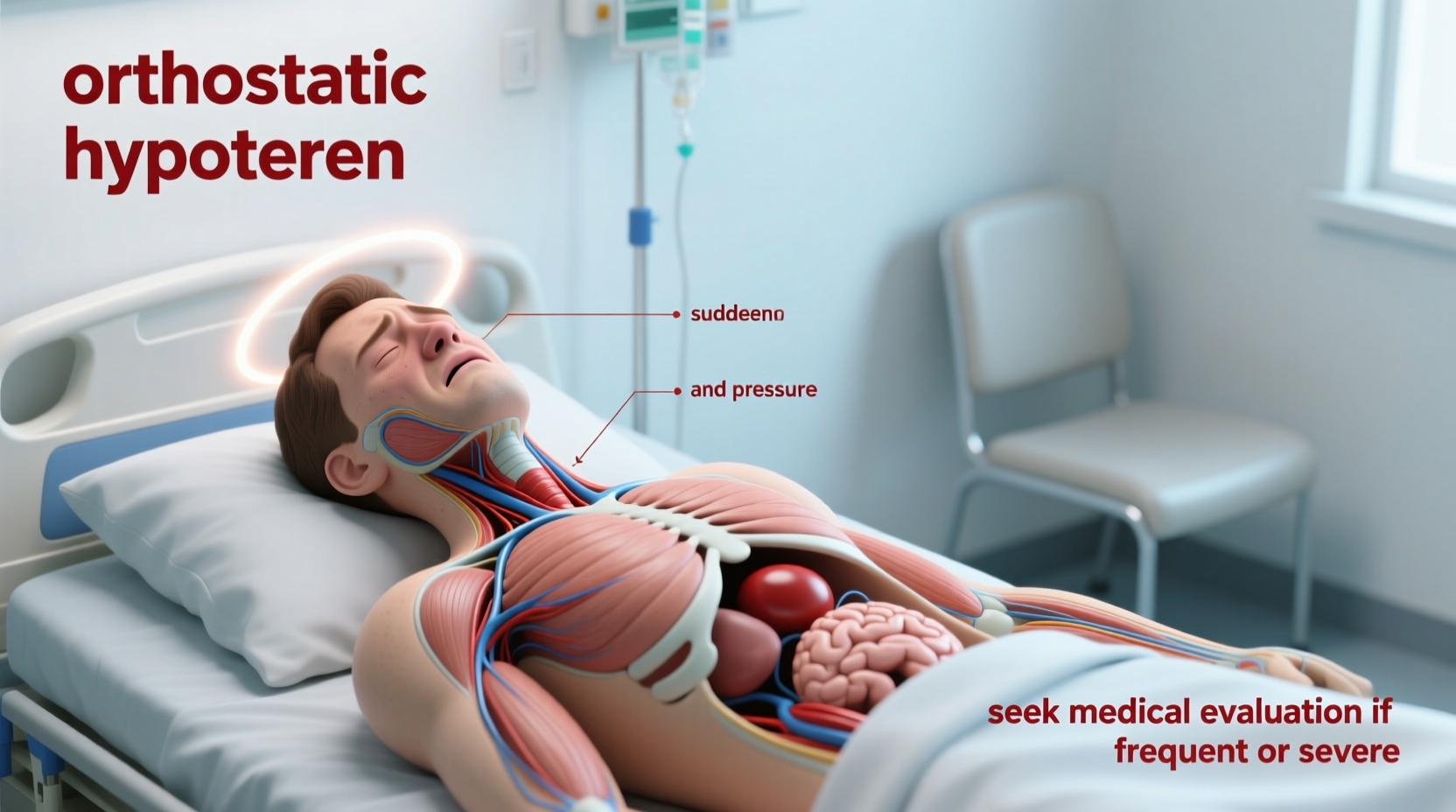
When you shift from sitting or lying down to standing, gravity pulls blood downward into your legs and abdomen. In healthy individuals, the body compensates almost instantly: blood vessels constrict, heart rate increases slightly, and blood pressure remains stable to ensure consistent cerebral perfusion. However, if this autonomic reflex is delayed or impaired, blood pressure falls temporarily, leading to reduced oxygen delivery to the brain and eyes—resulting in blurred vision, lightheadedness, or tunnel vision.
This transient drop in blood pressure is typically brief, lasting only seconds, and resolves once circulation stabilizes. The visual disturbances stem from retinal and optic nerve sensitivity to oxygen fluctuations. Even a small reduction in blood flow can disrupt normal visual processing in the occipital lobe, causing temporary blurring or dimming of sight.
Common Causes of Postural Vision Changes
Several physiological and environmental factors contribute to episodes of blurred vision upon standing. Some are benign and easily managed; others may point to deeper systemic concerns.
- Dehydration: Low fluid volume reduces circulating blood, making it harder for the body to maintain pressure during posture shifts.
- Medications: Diuretics, antihypertensives, antidepressants, and Parkinson’s drugs can interfere with vascular tone or heart rate regulation.
- Aging: Autonomic nervous system responsiveness declines with age, increasing susceptibility in older adults.
- Prolonged Bed Rest: Extended inactivity weakens circulatory adaptation, especially after illness or surgery.
- Dietary Deficiencies: Low salt intake, vitamin B12 deficiency, or anemia can impair red blood cell production and oxygen transport.
- Alcohol Consumption: Alcohol dilates blood vessels and dehydrates the body, amplifying postural instability.
In younger people, especially those with a lean build or naturally lower baseline blood pressure (e.g., athletes), occasional mild symptoms may be normal. However, frequency and severity matter. Recurrent or worsening episodes should prompt evaluation.
When to Be Concerned: Red Flags That Warrant Medical Attention
Occasional, fleeting blurriness upon standing is usually not dangerous. But certain signs suggest the need for prompt medical assessment. Ignoring persistent symptoms could delay diagnosis of conditions such as autonomic neuropathy, cardiac dysfunction, or endocrine disorders.
“Orthostatic symptoms shouldn’t be dismissed as ‘just getting older.’ Persistent dizziness on standing can be an early marker of neurodegenerative disease or heart failure.” — Dr. Lena Torres, Neurologist and Autonomic Specialist at Boston General Hospital
Seek medical advice if you experience any of the following:
- Frequent or worsening episodes (more than twice a week)
- Syncope (fainting) or near-fainting spells
- Chest pain, palpitations, or irregular heartbeat during episodes
- Nausea, confusion, or difficulty speaking alongside vision changes
- Symptoms occurring even after slow rising or while sitting upright
- History of diabetes, Parkinson’s, or heart disease
These indicators may reflect serious underlying pathology, including adrenal insufficiency, arrhythmias, or autonomic failure.
Step-by-Step Guide to Managing and Preventing Episodes
For most individuals, proactive lifestyle adjustments significantly reduce or eliminate postural vision disturbances. Follow this timeline-based approach to improve stability and minimize risk.
- Immediate Action (During an Episode): If you feel your vision blurring or become dizzy upon standing, stop moving. Sit or lie back down immediately. Lowering your head below heart level—by bending forward or lying flat—can restore cerebral blood flow within seconds.
- Short-Term Adjustment (Next 24–72 Hours): Increase fluid intake (aim for 1.5–2 liters daily unless contraindicated). Add modest amounts of salt to meals if blood pressure is normally low. Avoid hot environments, prolonged standing, and alcohol.
- Moderate-Term Strategy (1–4 Weeks): Monitor symptoms using a symptom diary. Record time of day, activity, food/drink consumed, medications, and episode severity. This data helps clinicians identify patterns.
- Long-Term Prevention (Ongoing): Incorporate compression stockings (15–20 mmHg) to prevent blood pooling in legs. Perform counter-pressure maneuvers like crossing legs and squeezing thighs when standing. Engage in regular aerobic exercise to enhance vascular tone.
- Medical Follow-Up (As Needed): Schedule a visit with your primary care physician or cardiologist if symptoms persist despite self-care. Request orthostatic vital signs testing—measuring blood pressure and heart rate lying, sitting, and standing at 1- and 3-minute intervals.
Do’s and Don’ts: Quick Reference Table
| Do’s | Don’ts |
|---|---|
| Rise slowly from bed or chair | Stand up abruptly after lying down |
| Stay well-hydrated throughout the day | Go hours without drinking fluids |
| Wear compression socks if advised | Wear tight waistbands that restrict circulation |
| Review medications with your doctor | Assume all dizziness is “normal” |
| Exercise regularly (walking, swimming) | Engage in heavy straining or Valsalva maneuvers |
Real-Life Example: Recognizing a Hidden Condition
Mark, a 58-year-old office worker, began noticing frequent blurriness when standing from his desk chair. Initially dismissing it as fatigue, he eventually fainted during a morning meeting. After being evaluated in urgent care, orthostatic testing revealed a 30-point drop in systolic blood pressure upon standing. Further investigation uncovered undiagnosed type 2 diabetes with early autonomic neuropathy—a complication affecting nerve signals that regulate blood vessel constriction.
With improved glucose control, increased hydration, and wearing compression garments, Mark’s symptoms resolved within three months. His case illustrates how seemingly minor visual disturbances can serve as critical warning signs of systemic disease.
FAQ: Common Questions About Vision Blurring When Standing
Is it normal to see spots or darkness when standing up?
Seeing dark spots or \"graying out\" briefly upon standing is relatively common, especially if done quickly. It's typically due to a temporary drop in blood pressure. However, if these episodes happen frequently, last longer than 5 seconds, or are accompanied by other symptoms like nausea or chest pain, they warrant medical evaluation.
Can anxiety cause blurred vision when standing?
Anxiety alone doesn’t directly cause postural vision changes, but it can amplify awareness of bodily sensations. Hyperventilation from anxiety may alter blood pH and reduce cerebral blood flow, potentially worsening dizziness. However, true orthostatic hypotension is measured objectively via blood pressure changes and requires clinical confirmation.
Why do I feel worse in the morning when I get up?
Morning episodes are common because overnight fasting and reduced fluid intake lower blood volume. Additionally, natural cortisol levels—which help maintain blood pressure—are lowest in the early hours. Rising slowly and hydrating first thing can mitigate this effect.
Expert Recommendations for Long-Term Monitoring
Healthcare providers emphasize patient education and early intervention. According to the American Heart Association, routine screening for orthostatic hypotension should be part of annual exams for adults over 65, particularly those on multiple medications or with chronic illnesses.
Dr. Alan Zhou, a cardiologist specializing in syncope management, advises: “Patients often don’t report these symptoms unless asked directly. We encourage open dialogue about dizziness and vision changes—they’re not just nuisances, but potential windows into cardiovascular and neurological health.”
“Early detection of orthostatic intolerance can prevent falls, fractures, and hospitalizations.” — American Academy of Neurology Clinical Guideline, 2023
Conclusion: Take Control of Your Health Today
Blurred vision when standing up suddenly is often manageable with simple lifestyle changes. Yet, when ignored or misattributed to stress or aging, it can mask serious health conditions. By understanding the causes, tracking symptoms, and knowing when to seek help, you empower yourself to act early and protect your long-term well-being.
If you’ve experienced repeated episodes—even if they seem minor—don’t hesitate to discuss them with your doctor. A quick blood pressure test could uncover a treatable issue. Small adjustments today can prevent significant complications tomorrow.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?