Vaginal discharge is a natural and essential part of the female reproductive system. Often described as mucus-like, this fluid helps keep the vagina clean, lubricated, and protected from infection. While most variations in discharge are completely normal, changes in color, smell, texture, or frequency can sometimes signal an underlying issue. Understanding what’s typical—and what isn’t—empowers individuals to monitor their reproductive health with confidence.
The consistency, volume, and appearance of vaginal mucus change throughout the menstrual cycle due to fluctuations in estrogen and progesterone. These hormonal shifts influence cervical fluid production, which plays a crucial role in fertility and vaginal hygiene. However, not all mucus is related to ovulation or menstruation—some may indicate infections like bacterial vaginosis or yeast overgrowth. Distinguishing between physiological (normal) and pathological (abnormal) discharge is key to maintaining long-term wellness.
Understanding Cervical Mucus: The Body’s Natural Lubricant
Cervical mucus is produced by glands in the cervix and varies significantly during the menstrual cycle. Its primary functions include:
- Protecting the uterus from bacteria and pathogens
- Lubricating the vaginal canal
- Facilitating sperm transport during fertile windows
- Maintaining a balanced vaginal pH
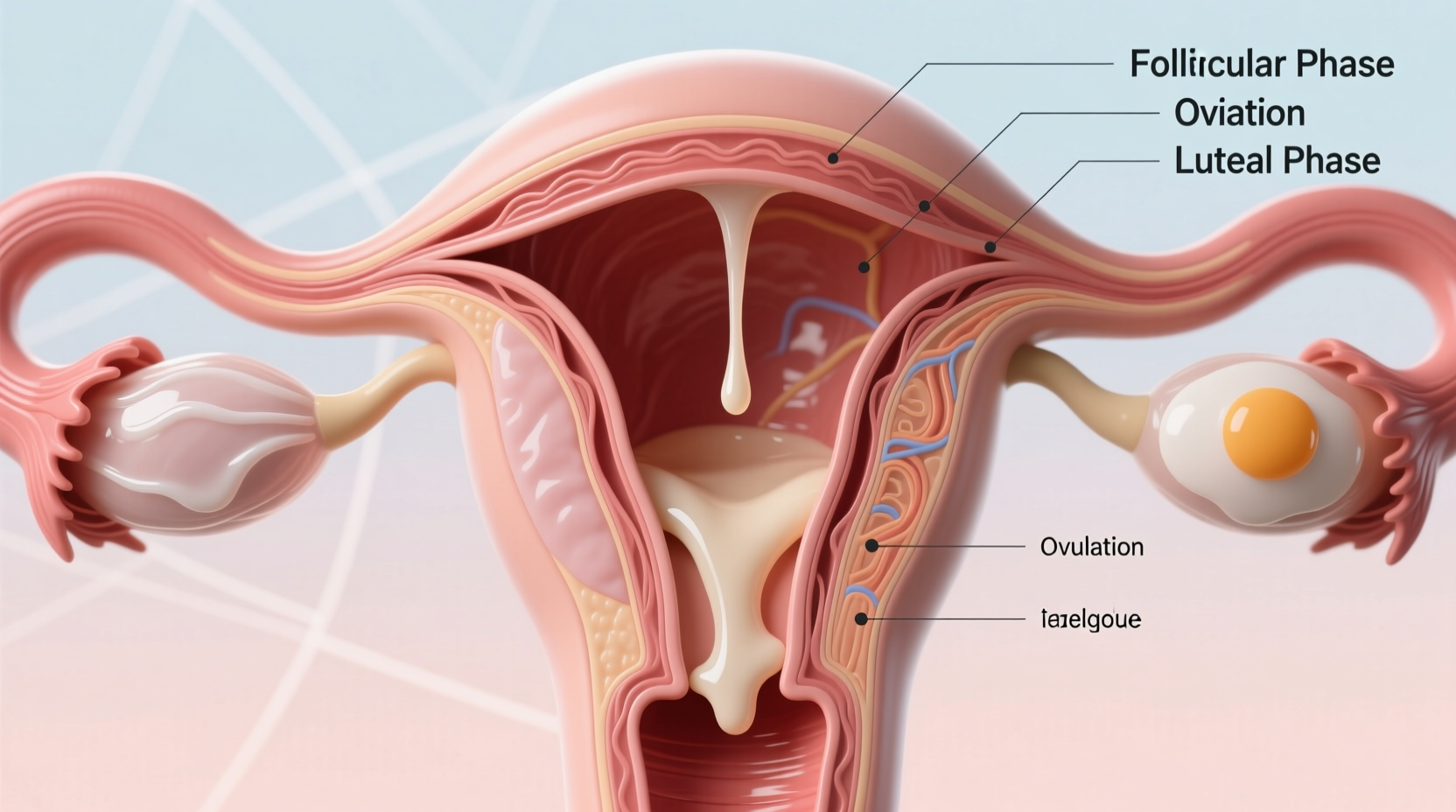
During the early follicular phase (just after menstruation), discharge is typically minimal and cloudy. As estrogen rises leading up to ovulation, mucus becomes more abundant, clear, and stretchy—often compared to raw egg white. This fertile-type mucus provides an optimal environment for sperm survival and movement. After ovulation, progesterone dominates, causing mucus to thicken, become sticky, and decrease in volume.
“Tracking cervical mucus patterns is one of the most reliable natural methods for identifying fertility windows.” — Dr. Lena Patel, OB-GYN and Reproductive Health Specialist
Normal vs. Abnormal Vaginal Mucus: What to Look For
Not all mucus is cause for concern. In fact, regular discharge is a sign of a healthy reproductive system. However, certain characteristics should prompt further evaluation.
| Characteristic | Normal | Abnormal |
|---|---|---|
| Color | Clear, white, or off-white | Yellow, green, gray, or bloody (outside period) |
| Odor | Mild or no odor | Strong fishy, sour, or foul smell |
| Texture | Slippery, stretchy, creamy, or dry depending on cycle | Thick, clumpy (like cottage cheese), frothy, or foamy |
| Accompanying Symptoms | None or mild wetness | Itching, burning, redness, swelling, pain, or discomfort |
For example, a sudden shift from clear, stretchy mucus to thick, white clumps with intense itching likely indicates a yeast infection. Conversely, grayish discharge with a fishy odor—especially after sex—is commonly associated with bacterial vaginosis (BV).
Common Causes of Vaginal Mucus Changes
Several factors influence the type and amount of mucus you experience. Some are entirely natural; others may require medical attention.
Hormonal Fluctuations
Ovulation, pregnancy, birth control use, perimenopause, and stress all affect hormone levels, directly impacting cervical fluid. Women on hormonal contraceptives often notice reduced or altered discharge due to suppressed ovulation.
Infections
Bacterial vaginosis, yeast infections, and sexually transmitted infections (STIs) such as trichomoniasis or chlamydia can alter mucus characteristics. Trichomoniasis, for instance, often causes yellow-green, frothy discharge with a strong odor.
Pregnancy
Increased blood flow and cervical stimulation during pregnancy lead to higher discharge volume. Known as leukorrhea, this thin, milky-white mucus is protective and typically harmless unless accompanied by irritation or odor.
Hygiene Practices
Douching, scented soaps, laundry detergents, and tight synthetic underwear can disrupt the vaginal microbiome, leading to irritation and abnormal mucus production. The vagina is self-cleaning—external washing with water is usually sufficient.
Medications and Antibiotics
Antibiotics can kill beneficial lactobacilli bacteria in the vagina, allowing yeast overgrowth and resulting in thick, white discharge. Similarly, antihistamines or hormonal treatments may reduce natural lubrication.
Mini Case Study: Recognizing a Yeast Infection Early
Sophia, a 29-year-old teacher, noticed her usual mid-cycle mucus had changed. Instead of clear and slippery, she observed thick, white clumps in her underwear, along with persistent itching. She recalled starting a new antibiotic for a sinus infection two weeks prior—a known risk factor for yeast overgrowth. Without waiting for symptoms to worsen, Sophia contacted her healthcare provider, who confirmed a candidiasis diagnosis through a simple swab test. She was prescribed antifungal treatment and advised to wear cotton underwear and avoid douching. Within days, her symptoms resolved, and normal mucus returned.
This case highlights the importance of recognizing deviations from personal norms and acting promptly—especially when lifestyle or medication changes coincide with symptoms.
Step-by-Step Guide to Monitoring Vaginal Health
Being proactive about vaginal mucus can help detect issues before they escalate. Follow this timeline to track and assess your discharge effectively:
- Day 1–7 (Menstruation): Expect blood mixed with mucus. Toward the end, you may see darker, sticky residue.
- Day 8–12 (Pre-Ovulation): Discharge increases, becoming cloudy or creamy. This signals rising estrogen.
- Day 13–15 (Ovulation): Look for clear, stretchy, egg-white-like mucus. This is your fertile window.
- Day 16–28 (Luteal Phase): Mucus thickens, turns sticky or pasty, then dries up. PMS symptoms may begin.
- Anytime – Red Flags: If you notice foul odor, unusual color, or discomfort, schedule a clinical evaluation. Do not self-diagnose STIs.
Frequently Asked Questions
Is it normal to have discharge every day?
Yes. Most people with vaginas produce some level of discharge daily. Volume and texture vary by cycle phase, but consistent, odorless, non-irritating mucus is generally healthy.
Can stress affect my vaginal mucus?
Absolutely. Chronic stress impacts cortisol and sex hormone balance, potentially altering mucus production and vaginal pH. This can increase susceptibility to infections.
When should I see a doctor about vaginal mucus?
Seek medical advice if you experience: persistent itching, burning, strong odor, pelvic pain, painful urination, or mucus that’s green, yellow, gray, or bloody without menstruation.
Actionable Checklist for Vaginal Wellness
- ✔️ Monitor daily discharge appearance and sensation
- ✔️ Avoid douching and scented feminine products
- ✔️ Wear breathable cotton underwear
- ✔️ Change tampons/pads regularly during periods
- ✔️ Stay hydrated and maintain a balanced diet
- ✔️ Practice safe sex and get routine STI screenings
- ✔️ Consult a healthcare provider for persistent or concerning changes
“The vagina has its own ecosystem. Interfering with it unnecessarily—like using fragranced washes—can do more harm than good.” — Dr. Amara Singh, Gynecologist and Microbiome Researcher
Conclusion
Vaginal mucus is not just normal—it’s a vital indicator of reproductive and overall health. By learning what’s typical for your body, you gain insight into your fertility, hormonal balance, and potential infections. While many fluctuations are harmless and cyclical, persistent changes in color, smell, or comfort warrant professional assessment. Empower yourself with knowledge, practice gentle care, and never hesitate to seek medical guidance when something feels off.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?