Hoarseness that lingers for days often prompts concern—especially when you haven’t been shouting or singing at concerts. While vocal strain from overuse is a frequent culprit, persistent changes in your voice can point to deeper health issues. The human voice relies on delicate coordination between the lungs, vocal cords, and surrounding tissues. When any part of this system becomes irritated, inflamed, or compromised, your tone may become raspy, weak, or even disappear entirely.
Understanding why your voice remains hoarse for days—even without obvious triggers—can help you take timely action. Some causes are minor and resolve with rest; others require medical evaluation to prevent long-term damage. This article explores the full spectrum of potential reasons behind prolonged hoarseness, offering practical insights into diagnosis, recovery, and prevention.
Common Causes of Prolonged Hoarseness
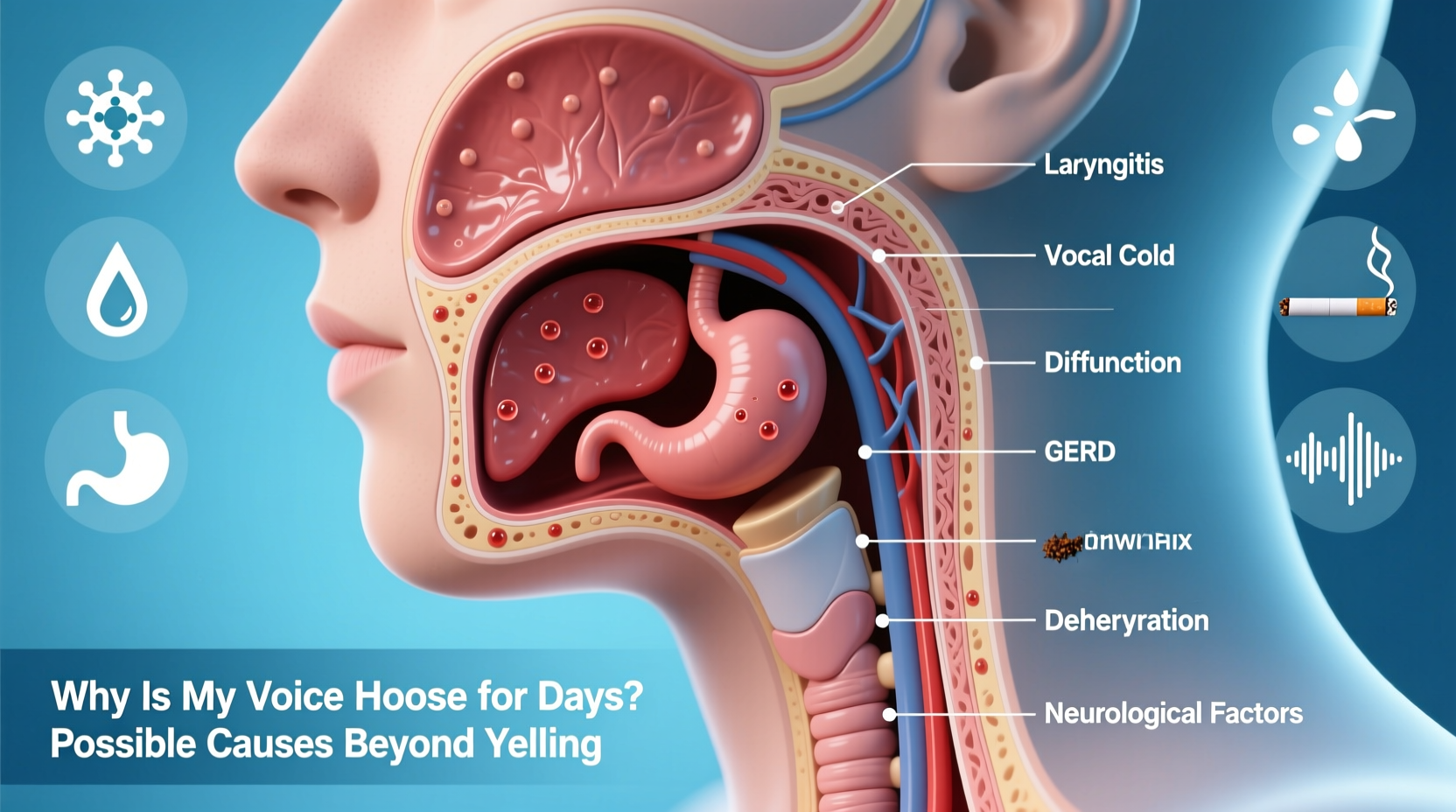
Vocal fatigue from yelling is well known, but many people underestimate how easily the voice can be affected by non-mechanical factors. The following conditions are among the most frequent contributors to hoarseness lasting more than a few days:
- Viral upper respiratory infections: Colds and flu cause inflammation in the larynx (voice box), leading to temporary hoarseness. Even after other symptoms fade, vocal irritation may persist for several days.
- Laryngitis: Inflammation of the vocal cords, whether viral or bacterial, disrupts normal vibration and alters pitch and clarity. Acute laryngitis typically resolves within two weeks, but chronic cases last longer.
- Acid reflux (LPR): Laryngopharyngeal reflux, also known as \"silent reflux,\" occurs when stomach acid travels up the esophagus and reaches the throat. Unlike typical heartburn, LPR often lacks chest pain but irritates the vocal folds directly.
- Allergies and postnasal drip: Mucus dripping down the back of the throat creates constant irritation, prompting throat clearing—a habit that further traumatizes the vocal cords.
- Dehydration: Vocal cords require adequate lubrication to function smoothly. Insufficient fluid intake leads to dryness and increased friction during speech.
Serious Medical Conditions Linked to Chronic Hoarseness
When hoarseness persists beyond three weeks, it should not be ignored. According to the American Academy of Otolaryngology–Head and Neck Surgery, chronic hoarseness warrants evaluation by an ENT specialist (otolaryngologist) to rule out structural or systemic disease.
Vocal Cord Nodules, Polyps, and Cysts
These benign growths develop due to repetitive trauma—often from poor vocal technique, chronic throat clearing, or excessive talking. Singers, teachers, and customer service professionals are particularly vulnerable.
- Nodules: Callus-like thickenings on both vocal cords, usually symmetrical.
- Polyps: Fluid-filled lesions that may appear on one cord, often larger than nodules.
- Cysts: Encapsulated masses beneath the surface layer of the cord.
All can distort vocal cord closure and lead to breathiness, strain, or reduced range.
Neurological Disorders
The vocal cords rely on precise nerve signaling from the brainstem via the vagus and recurrent laryngeal nerves. Damage or compression can result in vocal fold paralysis or paresis.
Conditions such as Parkinson’s disease, multiple sclerosis, or stroke may impair motor control of the larynx. Even thyroid surgery carries a risk of nerve injury, sometimes causing sudden hoarseness post-operation.
“Persistent hoarseness lasting more than two to three weeks should prompt evaluation with laryngoscopy. Early detection of vocal fold lesions or neurological causes improves outcomes significantly.” — Dr. Lena Patel, Laryngologist at Boston Voice Center
Thyroid Dysfunction
An underactive thyroid (hypothyroidism) can cause swelling of the vocal cords due to mucopolysaccharide deposition in the lamina propria—the soft tissue layer beneath the surface. Patients often report a deepened, sluggish voice alongside fatigue and weight gain.
Laryngeal Cancer
While less common, cancer of the larynx must be considered in individuals over 50 who smoke, drink heavily, or have persistent hoarseness. Early signs include:
- Unilateral vocal cord immobility
- Pain radiating to the ear
- Difficulty swallowing
- A sensation of a lump in the throat (globus pharyngeus)
Biopsy and imaging are essential for definitive diagnosis.
Environmental and Lifestyle Triggers
Beyond illness and anatomy, daily habits and surroundings play a major role in vocal health. Many people unknowingly expose their voices to damaging conditions.
| Factor | Impact on Voice | What You Can Do |
|---|---|---|
| Dry indoor air | Causes dehydration of mucous membranes | Use a humidifier, especially in winter |
| Smoking or secondhand smoke | Irritates laryngeal tissue and increases cancer risk | Quit smoking; avoid smoky environments |
| Excessive throat clearing | Creates microtrauma with each impact | Replace with gentle sipping or swallowing |
| Vocal overuse (e.g., teaching, call centers) | Leads to muscle tension and nodules | Take vocal naps; use amplification if needed |
| Spicy or acidic foods | Triggers silent reflux affecting the throat | Limit intake, especially before bedtime |
Real-Life Example: A Teacher’s Journey with Chronic Hoarseness
Maria, a 47-year-old high school English teacher, noticed her voice becoming increasingly strained each semester. She attributed it to classroom demands—projecting over students, grading aloud, attending meetings. For years, she pushed through, using lozenges and tea to soothe her throat.
After a particularly rough winter, her hoarseness lasted nearly six weeks. Concerned, she visited an ENT specialist. A flexible laryngoscopy revealed bilateral vocal nodules—callus-like growths from years of vocal misuse. The doctor explained that compensatory strain had worsened the condition.
Maria began working with a speech-language pathologist specializing in voice therapy. Over eight weeks, she learned resonant voice techniques, proper breath support, and strategies to reduce throat clearing. She also started using a personal microphone in class. Within three months, her voice improved dramatically. Follow-up imaging showed significant reduction in nodule size.
Her case underscores a key truth: occupational voice users need proactive care, not just reactive fixes.
When to See a Doctor: A Step-by-Step Guide
Not every hoarse voice requires urgent attention—but knowing when to seek help prevents complications. Follow this timeline to assess your situation:
- Days 1–3: Monitor symptoms. Rest your voice, hydrate, and avoid irritants like smoke or alcohol. Most mild cases resolve here.
- Day 4–7: If hoarseness persists, consider recent illnesses, allergies, or reflux. Try antihistamines (if allergic) or an antacid trial (for suspected LPR).
- Week 2: No improvement? Schedule an appointment with your primary care provider. They may refer you to an ENT.
- Week 3+: Persistent hoarseness now qualifies as “chronic.” An otolaryngologist should perform a laryngoscopy to visualize the vocal cords directly.
- Immediate red flags: Seek care right away if you experience pain, difficulty breathing, coughing up blood, or complete voice loss without clear cause.
Prevention Checklist: Protect Your Voice Daily
Maintaining vocal health is both preventive and cumulative. Use this checklist to build sustainable habits:
- ✅ Stay well-hydrated—aim for 6–8 glasses of water daily
- ✅ Use a humidifier in dry climates or heated rooms
- ✅ Avoid yelling, whispering, or speaking over loud noise
- ✅ Practice good posture to support breath control
- ✅ Limit caffeine and alcohol, especially before speaking engagements
- ✅ Quit smoking and minimize exposure to airborne irritants
- ✅ Treat allergies and reflux promptly
- ✅ Take short “vocal naps” during long speaking periods
- ✅ Learn proper vocal technique if you use your voice professionally
- ✅ Get evaluated early if hoarseness lasts more than three weeks
Frequently Asked Questions
Can allergies really make my voice hoarse for days?
Yes. Allergic reactions increase mucus production and postnasal drip, which irritates the throat lining. Frequent throat clearing aggravates the vocal cords, prolonging hoarseness even after the allergy flare subsides. Treating the underlying allergy with antihistamines or nasal steroids often resolves the issue.
Is whispering better than talking when my voice is hoarse?
No. Whispering actually strains the vocal cords more than soft speech. It forces the arytenoid cartilages to press together tightly while allowing turbulent airflow, creating irritation. Instead, speak softly using normal vocal tone, or rest your voice completely.
How does acid reflux affect my voice without heartburn?
Laryngopharyngeal reflux (LPR) allows small amounts of stomach acid to reach the throat, especially at night. Because the larynx is highly sensitive, even微量 acid exposure causes swelling and inflammation. Many patients don’t feel classic heartburn but notice morning hoarseness, throat tightness, or a need to constantly clear their throat.
Conclusion: Listen to Your Voice—It’s Telling You Something
Your voice is more than a tool for communication—it's a window into your overall health. Persistent hoarseness lasting days or weeks is not something to dismiss as mere fatigue. Whether caused by infection, lifestyle habits, or a more serious condition, prolonged voice changes deserve attention.
Early intervention preserves vocal function and rules out dangerous pathologies. Simple measures like hydration, vocal rest, and environmental adjustments go a long way. But when symptoms linger, professional evaluation isn't optional—it's essential.
Treat your voice with the care it deserves. After all, it speaks for you every day.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?