In vitro fertilization (IVF) has revolutionized reproductive medicine, offering hope to millions struggling with infertility. Since the birth of the first IVF baby in 1978, over 8 million children have been born using this technology. Despite its success, IVF is not without significant risks, emotional tolls, financial burdens, and ethical dilemmas. For many individuals and couples, the decision to pursue IVF involves weighing these substantial drawbacks against the desire for biological parenthood. Understanding the full scope of what IVF entails—beyond the promise of a positive pregnancy test—is essential for making informed, realistic choices.
Physical Health Risks and Medical Complications
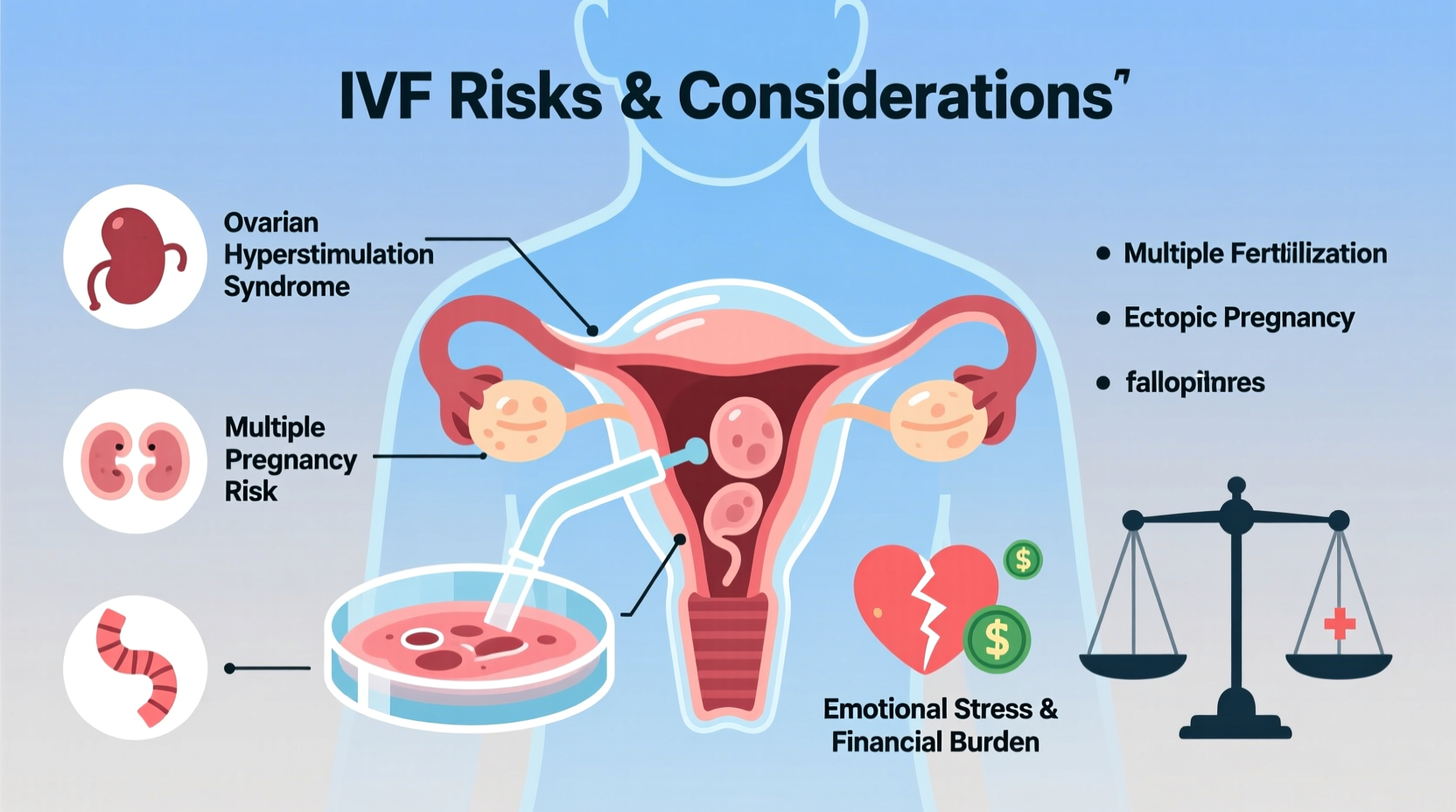
IVF involves a series of medical procedures that place considerable stress on the female body. The process begins with ovarian stimulation, where hormone injections are used to produce multiple eggs in a single cycle. While effective, this phase carries several health risks.
One of the most common complications is Ovarian Hyperstimulation Syndrome (OHSS), which affects up to 10% of women undergoing IVF. Symptoms range from mild bloating and nausea to severe fluid accumulation in the abdomen and chest, requiring hospitalization in extreme cases. In rare instances, OHSS can lead to blood clots, kidney failure, or even death.
The egg retrieval procedure itself, though minimally invasive, poses risks such as infection, bleeding, and damage to surrounding organs like the bowel or bladder. Additionally, IVF increases the likelihood of multiple pregnancies when more than one embryo is transferred. Multiple gestations significantly raise the risk of preterm birth, low birth weight, preeclampsia, and long-term developmental issues for infants.
“While IVF offers a path to conception, it’s critical to recognize that it’s not a benign procedure. The hormonal manipulation and surgical aspects carry real, sometimes serious, health consequences.” — Dr. Rachel Nguyen, Reproductive Endocrinologist, Mayo Clinic
Emotional and Psychological Toll
The emotional burden of IVF is often underestimated. The process is grueling—marked by daily injections, frequent monitoring appointments, and the constant anticipation of results. Each stage brings new anxiety: Will the ovaries respond? Will enough eggs mature? Will fertilization occur? Will the embryo implant?
Studies show that women undergoing IVF report stress levels comparable to those diagnosed with cancer or heart disease. The repetitive cycle of hope and disappointment—with an average live birth rate per cycle of around 30% for women under 35, dropping sharply with age—can lead to depression, anxiety, and relationship strain.
Many patients describe feeling isolated, especially when friends or family conceive easily. Social events centered around children can become painful reminders of unfulfilled dreams. The pressure to succeed, combined with the physical discomfort of treatment, often leads to burnout, with some abandoning treatment altogether after two or three failed cycles.
Mini Case Study: Sarah and James
Sarah, 38, and James, 41, tried for five years to conceive naturally and through intrauterine insemination (IUI) before turning to IVF. They invested $22,000 in their first cycle, only to receive a negative beta test. The second cycle resulted in a chemical pregnancy. By the third attempt, Sarah was experiencing panic attacks before blood tests and had withdrawn from social circles. After another failed transfer, they paused treatment to focus on counseling. Their story reflects the silent psychological crisis many face—where the pursuit of parenthood begins to erode mental well-being.
Financial Burden and Accessibility Issues
IVF is notoriously expensive. A single cycle in the United States averages between $12,000 and $17,000—not including medications, which can add $3,000 to $5,000. Additional procedures like genetic testing (PGT-A), frozen embryo transfers, or donor eggs can push total costs over $25,000 per attempt.
Insurance coverage varies widely. Only 19 U.S. states mandate some form of IVF coverage, and even then, limits apply. Many patients must pay out-of-pocket, leading to debt, drained savings, or crowdfunding. The financial strain often forces difficult decisions—such as transferring multiple embryos to increase odds, thereby increasing health risks, or discontinuing treatment prematurely due to cost.
| Expense | Average Cost (USD) | Notes |
|---|---|---|
| IVF Cycle (base) | $12,000–$17,000 | Includes monitoring, retrieval, fertilization |
| Fertility Medications | $3,000–$5,000 | Vary by dosage and protocol |
| Genetic Testing (PGT-A) | $3,000–$7,000 | Per batch of embryos |
| Frozen Embryo Transfer (FET) | $3,000–$5,000 | Additional if needed |
| Total (First Full Attempt) | $20,000–$30,000+ | Often requires multiple attempts |
Ethical and Moral Considerations
IVF raises complex ethical questions that vary by personal, religious, and cultural beliefs. One major concern is the creation and fate of surplus embryos. Many IVF cycles produce more embryos than are transferred, leaving patients to decide whether to freeze them (incurring ongoing storage fees), donate them to research, give them to other couples, or discard them. For individuals with strong moral or religious convictions, these choices can be deeply distressing.
Another issue is the potential for selective reduction in multiple pregnancies—a procedure that involves terminating one or more fetuses to improve outcomes for the remaining ones. This can conflict with pro-life beliefs and cause lasting emotional trauma.
Additionally, the commercialization of reproduction—through egg donation, surrogacy, and international fertility tourism—raises concerns about exploitation, especially when economic disparities drive young women to sell their eggs for financial gain.
Success Rates and Realistic Expectations
One of the most misunderstood aspects of IVF is its actual success rate. Clinics often advertise high “take-home baby” rates, but these figures may be misleading. Success depends heavily on age, diagnosis, clinic protocols, and prior fertility history.
According to the CDC, the live birth rate per IVF cycle using a woman’s own eggs is:
- Under 35: ~55%
- 35–37: ~41%
- 38–40: ~26%
- 41–42: ~13%
- Over 42: ~4%
These numbers reflect ideal candidates. For those with diminished ovarian reserve, endometriosis, or unexplained infertility, success rates may be significantly lower. Yet, many patients enter treatment believing IVF is a guaranteed solution, only to face repeated disappointments.
Checklist: Key Questions Before Starting IVF
- Have I consulted a reproductive endocrinologist for a full diagnostic evaluation?
- Have I explored lower-cost alternatives (e.g., IUI, ovulation induction)?
- Do I understand the risks of OHSS, multiple births, and ectopic pregnancy?
- Can I afford one full cycle—and potentially multiple attempts—without financial hardship?
- Have I discussed emotional support options with my partner or a therapist?
- What is my clinic’s live birth rate per cycle for someone my age?
- Do I have a plan for unused embryos?
Frequently Asked Questions
Is IVF dangerous for the mother?
While generally safe, IVF carries medical risks such as OHSS, infection from egg retrieval, and complications from multiple pregnancies. Long-term studies suggest a possible slight increase in certain cancers, though evidence remains inconclusive. Close monitoring during treatment helps mitigate many risks.
Why does IVF fail so often?
Failure can result from poor egg or sperm quality, embryo chromosomal abnormalities, uterine receptivity issues, or undiagnosed immunological factors. Age is the strongest predictor—egg quality declines significantly after 35, reducing the chances of viable embryo development.
Are IVF babies less healthy?
Most IVF children are healthy, but studies indicate a slightly higher risk of birth defects, low birth weight, and preterm delivery compared to naturally conceived children. These risks are partly linked to underlying infertility and multiple births rather than the IVF process itself.
Conclusion: Making an Informed Decision
IVF is a powerful tool, but it is not a simple fix. It demands physical resilience, emotional endurance, financial readiness, and thoughtful reflection on ethical boundaries. For some, it leads to the joy of parenthood. For others, it brings profound loss and exhaustion. Recognizing the risks and limitations doesn’t diminish its value—it empowers patients to approach treatment with eyes wide open.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?