Blood transfusions are one of modern medicine’s most vital interventions. They can mean the difference between life and death in critical situations, support recovery during surgery, and help manage long-term medical conditions. Every year, millions of people worldwide receive transfusions to replace lost or deficient blood components. While many associate transfusions with accidents or emergencies, they are also essential for treating chronic illnesses, supporting cancer therapies, and managing complications during childbirth. Understanding why a transfusion might be necessary empowers patients to ask informed questions and reduces anxiety around the procedure.
What Is a Blood Transfusion?
A blood transfusion is a medical procedure where donated blood or specific blood components—such as red blood cells, platelets, plasma, or cryoprecipitate—are introduced into a patient’s bloodstream through an intravenous (IV) line. The type of transfusion depends on what the patient lacks. For example, someone bleeding heavily may need red blood cells, while a person with a clotting disorder might require plasma or platelets.
Before transfusion, blood is carefully matched to the recipient’s blood type to prevent adverse reactions. The process typically takes 1 to 4 hours depending on the volume and component being administered. Most patients tolerate transfusions well, though monitoring is standard to catch any rare complications early.
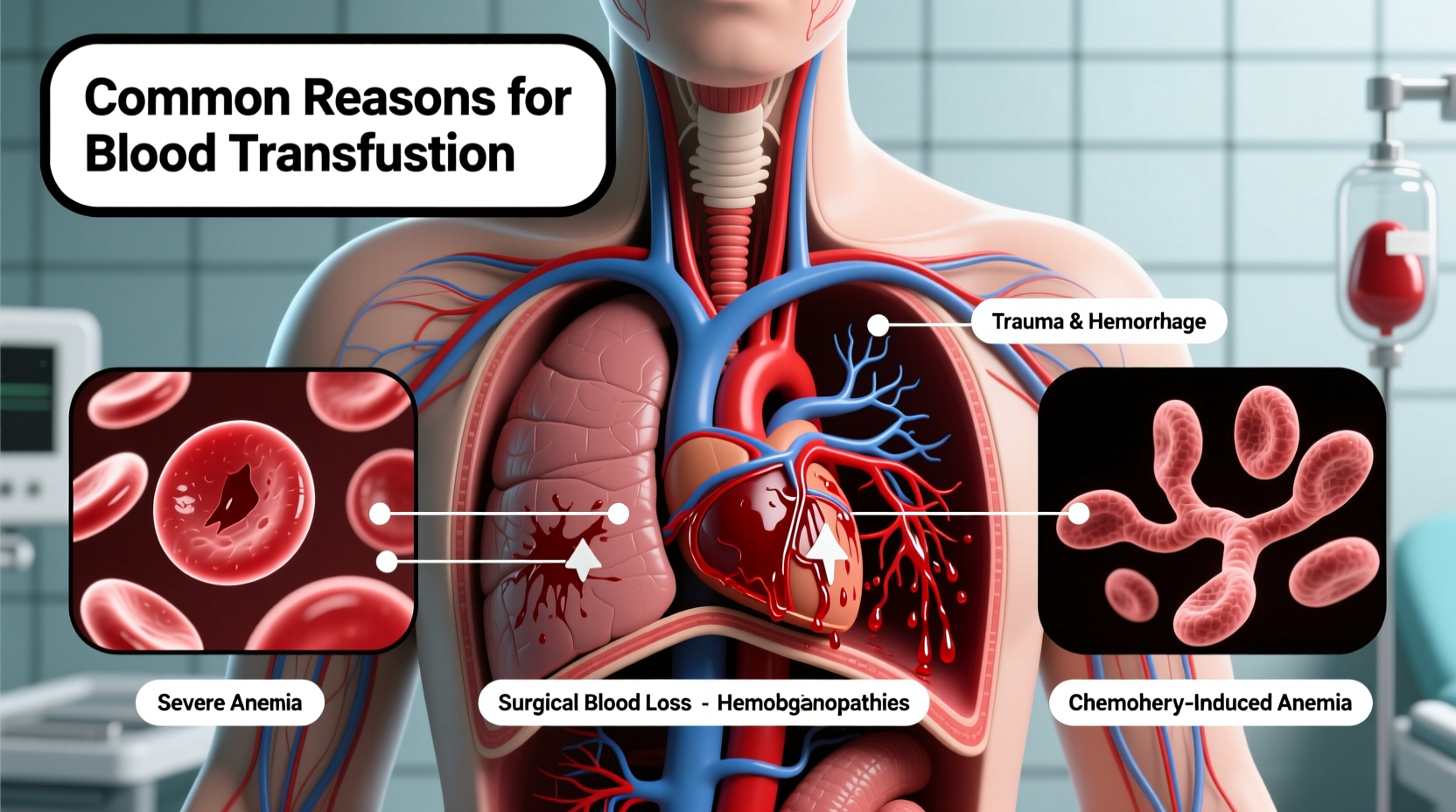
Major Medical Reasons for Blood Transfusions
Transfusions are not performed lightly. Doctors evaluate hemoglobin levels, symptoms, and clinical context before recommending one. Below are some of the most common scenarios in which a transfusion becomes medically necessary.
1. Severe Blood Loss from Trauma or Surgery
Sudden, significant blood loss is one of the leading reasons for emergency transfusions. Accidents, gunshot wounds, or major surgeries—especially those involving the abdomen, heart, or spine—can result in rapid depletion of blood volume. When more than 30% of total blood is lost, the body struggles to deliver oxygen to vital organs, risking shock and organ failure.
In such cases, transfusions restore circulating volume and oxygen-carrying capacity. Trauma centers maintain ready supplies of O-negative blood—the universal donor type—for immediate use when there’s no time to cross-match.
2. Anemia Requiring Rapid Correction
Anemia—a condition marked by low red blood cell count or hemoglobin—can develop gradually or acutely. While mild anemia is often managed with iron, vitamins, or medications, severe cases may require transfusion, especially if symptoms like chest pain, shortness of breath, or dizziness occur.
Common causes of transfusion-requiring anemia include:
- Gastrointestinal bleeding (e.g., ulcers, diverticulosis)
- Heavy menstrual bleeding
- Chronic kidney disease (which impairs red blood cell production)
- Nutritional deficiencies unresponsive to supplementation
Transfusions provide immediate relief but don’t cure the underlying cause. Patients must undergo diagnostic testing to identify and treat the source of anemia.
3. Cancer and Chemotherapy Complications
Cancer patients frequently need transfusions due to both the disease and its treatment. Tumors, especially in the bone marrow (like leukemia), can disrupt normal blood cell production. Chemotherapy and radiation therapy further suppress bone marrow function, leading to anemia and thrombocytopenia (low platelets).
Regular monitoring of blood counts is standard during oncology care. When hemoglobin drops below 7–8 g/dL or symptoms worsen, a red blood cell transfusion may be given. Platelet transfusions are common when counts fall below 10,000/μL, particularly if fever or active bleeding is present.
“Transfusions are a lifeline for many cancer patients. They allow continuation of aggressive treatments that would otherwise be too taxing on the body.” — Dr. Lena Patel, Hematology Specialist
4. Blood Disorders Like Sickle Cell Disease and Thalassemia
Chronic blood disorders often necessitate lifelong transfusion regimens. In sickle cell disease, abnormal red blood cells become rigid and block blood flow, causing pain crises and organ damage. Regular transfusions reduce the percentage of sickled cells, lowering complication risks.
Similarly, thalassemia major patients cannot produce enough healthy hemoglobin and rely on frequent red blood cell transfusions from childhood. These transfusions sustain growth, prevent skeletal deformities, and improve quality of life.
However, long-term transfusion therapy carries risks like iron overload, requiring chelation therapy to remove excess iron from the body.
5. Complications During Pregnancy and Childbirth
Obstetric hemorrhage—excessive bleeding during or after delivery—is a leading cause of maternal mortality worldwide. It can result from placental abruption, uterine rupture, or retained placenta. When fluid resuscitation isn’t enough, blood transfusions are critical to stabilize the mother.
Women with pre-existing anemia, multiple pregnancies, or placenta previa are at higher risk. Hospitals routinely prepare blood products for high-risk deliveries. In emergencies, massive transfusion protocols activate to deliver multiple units rapidly.
Types of Blood Components Used in Transfusions
Not all transfusions involve whole blood. Modern medicine uses component therapy to target specific deficiencies. This approach maximizes donor blood utility and minimizes side effects.
| Component | Purpose | Common Conditions Treated |
|---|---|---|
| Red Blood Cells (RBCs) | Carry oxygen; treat anemia and blood loss | Trauma, surgery, chronic anemia |
| Platelets | Prevent or control bleeding | Chemotherapy, leukemia, dengue, ITP |
| Plasma | Provides clotting factors | Liver disease, warfarin overdose, DIC |
| Cryoprecipitate | Treats fibrinogen deficiency | Hemophilia A, von Willebrand disease |
Mini Case Study: Emergency Response Saves Life After Car Accident
James R., a 34-year-old construction worker, was involved in a high-speed collision. He arrived at the emergency department unconscious, with a ruptured spleen and dropping blood pressure. His initial hemoglobin was 5.8 g/dL—less than half the normal level. The trauma team initiated a massive transfusion protocol, administering 6 units of O-negative red blood cells, 4 units of plasma, and 1 unit of platelets within two hours.
After emergency surgery to control bleeding, James stabilized. Over the next week, he received two more RBC transfusions during recovery. Without timely blood products, his chances of survival would have been minimal. His case illustrates how coordinated access to blood can turn a fatal outcome into a full recovery.
Step-by-Step: What Happens During a Blood Transfusion
Understanding the process can ease concerns for first-time recipients. Here’s what typically occurs:
- Prescription and Consent: A doctor orders the transfusion and explains risks and benefits. Patient consent is obtained.
- Blood Typing and Crossmatching: A sample is tested to ensure compatibility with donor blood.
- Preparation: Blood is issued from the blood bank and double-checked by two medical staff members.
- Administration: An IV line is inserted, and the transfusion begins slowly (usually over 2–4 hours).
- Monitoring: Vital signs are checked frequently during the first 15 minutes and throughout.
- Completion and Observation: After infusion, the patient is monitored briefly for delayed reactions.
Most reactions occur within the first 15–30 minutes. Common signs include fever, chills, rash, or shortness of breath—prompt reporting allows immediate intervention.
Frequently Asked Questions
Are blood transfusions safe?
Yes, transfusions are extremely safe due to rigorous donor screening, infectious disease testing (HIV, hepatitis B/C, syphilis, etc.), and blood typing protocols. Serious complications are rare, affecting fewer than 1 in 100,000 units transfused.
Can I refuse a blood transfusion?
Yes, patients have the right to refuse treatment, including transfusions, based on personal, religious, or ethical beliefs. However, doctors will explain the risks of refusal, especially in life-threatening situations. Alternatives like erythropoietin or iron infusions may be considered when appropriate.
How long do transfused blood cells last?
Red blood cells typically survive about 120 days. Platelets last 3–7 days, and plasma proteins are replenished within days. Chronic patients may need repeat transfusions based on their condition.
Checklist: Before and After Your Transfusion
- ✔ Discuss your medical history and allergies with your care team
- ✔ Confirm your identity and blood type before the transfusion starts
- ✔ Report any itching, fever, or discomfort immediately
- ✔ Stay hydrated and rest after the procedure
- ✔ Attend follow-up appointments to monitor response and address underlying causes
Conclusion
Blood transfusions remain a cornerstone of effective medical care across countless conditions—from sudden trauma to lifelong diseases. Knowing the common reasons for transfusion helps demystify the process and underscores its importance in saving and sustaining lives. Advances in blood safety, component therapy, and patient monitoring continue to improve outcomes.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?