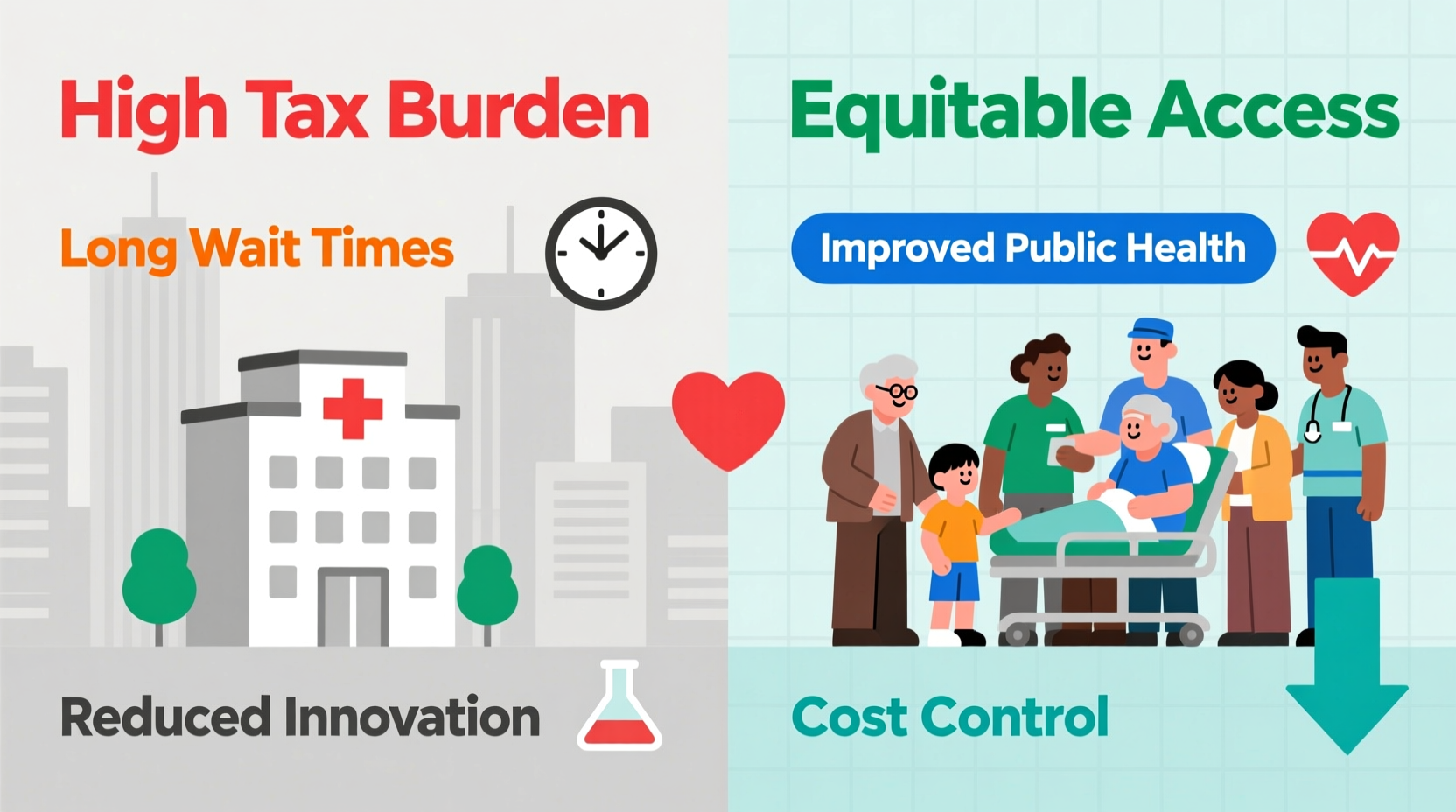
Universal healthcare—where all citizens receive medical services funded by the government—is often praised for promoting equity and access. However, it also raises serious concerns about cost, efficiency, and quality. While the intent behind universal systems is commendable, real-world implementation reveals significant drawbacks that affect economies, patient outcomes, and medical innovation. Understanding these criticisms is essential for informed public debate and policy development.
Economic Burden and Taxation Pressure
One of the most frequently cited arguments against universal healthcare is its financial impact on national budgets and taxpayers. Implementing and maintaining a nationwide system requires substantial public funding, typically drawn from increased taxation. Countries like Canada and the UK fund their systems through income, sales, and corporate taxes, placing a heavy burden on working individuals and businesses.
In 2023, the UK spent approximately £179 billion on the National Health Service (NHS), equating to over £6,000 per household annually. While this covers basic care, it leaves little room for investment in cutting-edge treatments or infrastructure upgrades without further tax hikes. High public spending on healthcare can crowd out funding for education, defense, and transportation.
Reduced Efficiency and Long Wait Times
A hallmark of many universal systems is delayed access to care. Because services are centrally managed and resources are limited, patients often face long wait times for non-emergency procedures. In Canada, the median wait time between referral by a general practitioner and treatment was 27.4 weeks in 2023, according to the Fraser Institute.
These delays aren’t merely inconvenient—they can be life-threatening. A patient with early-stage cancer may deteriorate while waiting for surgery or diagnostics. Similarly, chronic pain sufferers may experience reduced quality of life due to postponed specialist consultations.
“Timeliness is a critical component of effective healthcare. Delays in diagnosis and treatment directly correlate with poorer outcomes.” — Dr. Richard Anderson, Health Economist, University of Toronto
Common Procedures and Average Wait Times (Canada, 2023)
| Procedure | Average Wait Time (Weeks) |
|---|---|
| Orthopedic Surgery (e.g., hip/knee replacement) | 52.4 |
| Neurosurgery | 40.1 |
| MRI Scan | 11.6 |
| Radiation Therapy | 5.0 |
The lack of competition and price signals in monopolized systems reduces incentives for efficiency. Without market pressure to improve service speed or patient satisfaction, bureaucratic inertia becomes common.
Stifled Medical Innovation and Research
Universal healthcare systems often prioritize cost control over innovation. Governments acting as single payers negotiate low reimbursement rates, which disincentivizes pharmaceutical companies and medical device manufacturers from developing new treatments. The U.S., with its mixed-market system, accounts for nearly half of global medical R&D spending despite having only 4% of the world’s population.
When governments cap prices or restrict access to expensive therapies, companies shift focus away from high-risk research areas such as gene therapy or rare diseases. For example, some European countries delay or deny approval of breakthrough oncology drugs due to cost-effectiveness thresholds, limiting patient access compared to the U.S.
Additionally, doctors under universal systems may avoid adopting new technologies if they aren’t covered by public funding. This creates a cycle where innovation slows, and patients receive outdated standards of care.
Checklist: Evaluating the Impact of Universal Healthcare on Innovation
- Assess annual national investment in medical R&D
- Compare drug approval timelines between countries
- Review availability of novel treatments (e.g., CAR-T therapy)
- Analyze physician autonomy in prescribing advanced medications
- Monitor trends in private-sector biotech startups
Reduced Patient and Provider Autonomy
Under universal healthcare, both patients and physicians often lose decision-making power. Treatment options may be restricted based on government guidelines rather than individual needs. Doctors might be required to follow standardized protocols that don't account for patient-specific conditions.
For instance, the NHS uses the National Institute for Health and Care Excellence (NICE) to determine which drugs and procedures are “cost-effective.” If a treatment exceeds a certain cost-per-quality-adjusted-life-year (QALY) threshold, it may be denied—even if proven effective. This turns medical decisions into economic calculations.
Patient choice is also limited. Elective procedures, second opinions, or preferred specialists may not be available without paying out-of-pocket or traveling abroad. In essence, while care is “free” at the point of service, freedom of choice comes at a premium.
“In a system where bureaucrats decide what treatments are ‘worth’ providing, medicine risks becoming a spreadsheet exercise instead of a healing profession.” — Dr. Sarah Thompson, Former NHS Consultant
Real-World Example: The Case of Emma Wilson
Emma Wilson, a 58-year-old teacher from Manchester, was diagnosed with early-stage breast cancer in 2022. Her oncologist recommended a targeted therapy drug known to reduce recurrence risk by 40%. However, NICE had not approved the drug for routine use due to its high cost.
After appealing through her local clinical commissioning group, she waited four months for a decision—time during which her anxiety worsened and treatment was delayed. Ultimately, her request was denied. She raised funds privately to pay £12,000 for the treatment abroad, returning home weakened but hopeful.
Emma’s story highlights how cost containment can override personalized care. While the system protected public funds, it compromised patient agency and timely intervention.
Frequently Asked Questions
Does universal healthcare mean no one pays anything?
No. While services may appear “free” at delivery, citizens pay through taxes. In many cases, total lifetime contributions exceed what individuals would pay in premiums under private systems. Additionally, co-pays for prescriptions or dental care are common even in universal systems.
Can people opt out of universal healthcare?
In most countries, yes—but with limitations. In the UK, patients can purchase private insurance for faster access, but doing so doesn’t exempt them from contributing via taxes. This creates a dual burden: funding the public system while paying again for better care.
Are emergency services affected under universal healthcare?
Emergency care is generally prioritized and accessible quickly. However, overcrowding due to systemic inefficiencies can strain ERs. Ambulance response times in England hit record highs in 2023, with Category 2 responses averaging over 40 minutes—double the target time.
Conclusion: Balancing Access with Sustainability
Universal healthcare aims to ensure everyone receives medical attention regardless of income—a noble goal. Yet, its drawbacks cannot be ignored. From economic strain and long waits to stifled innovation and eroded autonomy, the model presents trade-offs that impact both quality and sustainability.
No system is perfect, but understanding the weaknesses allows policymakers and citizens to push for reforms that preserve access without sacrificing speed, innovation, or choice. Hybrid models—combining public coverage for essential services with private options for expedited or specialized care—may offer a more balanced path forward.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?