Tuberculosis (TB) remains a significant global health concern, with millions affected annually. One of the most widely used tools in TB screening is the purified protein derivative (PPD) skin test, also known as the Mantoux test. While simple in concept, its accuracy hinges on proper administration and, critically, correct interpretation. Misreading the test can lead to false positives or missed diagnoses, both of which carry serious clinical consequences. Understanding how to measure and interpret the induration—rather than redness—is essential for healthcare providers and patients alike.
Understanding the PPD Skin Test Procedure
The PPD test involves injecting 0.1 mL of tuberculin solution just beneath the top layer of skin on the forearm using a standardized intradermal technique. When performed correctly, this creates a small, pale bump called a bleb. The test must be read between 48 and 72 hours after administration; readings outside this window are unreliable due to fluctuating immune responses.
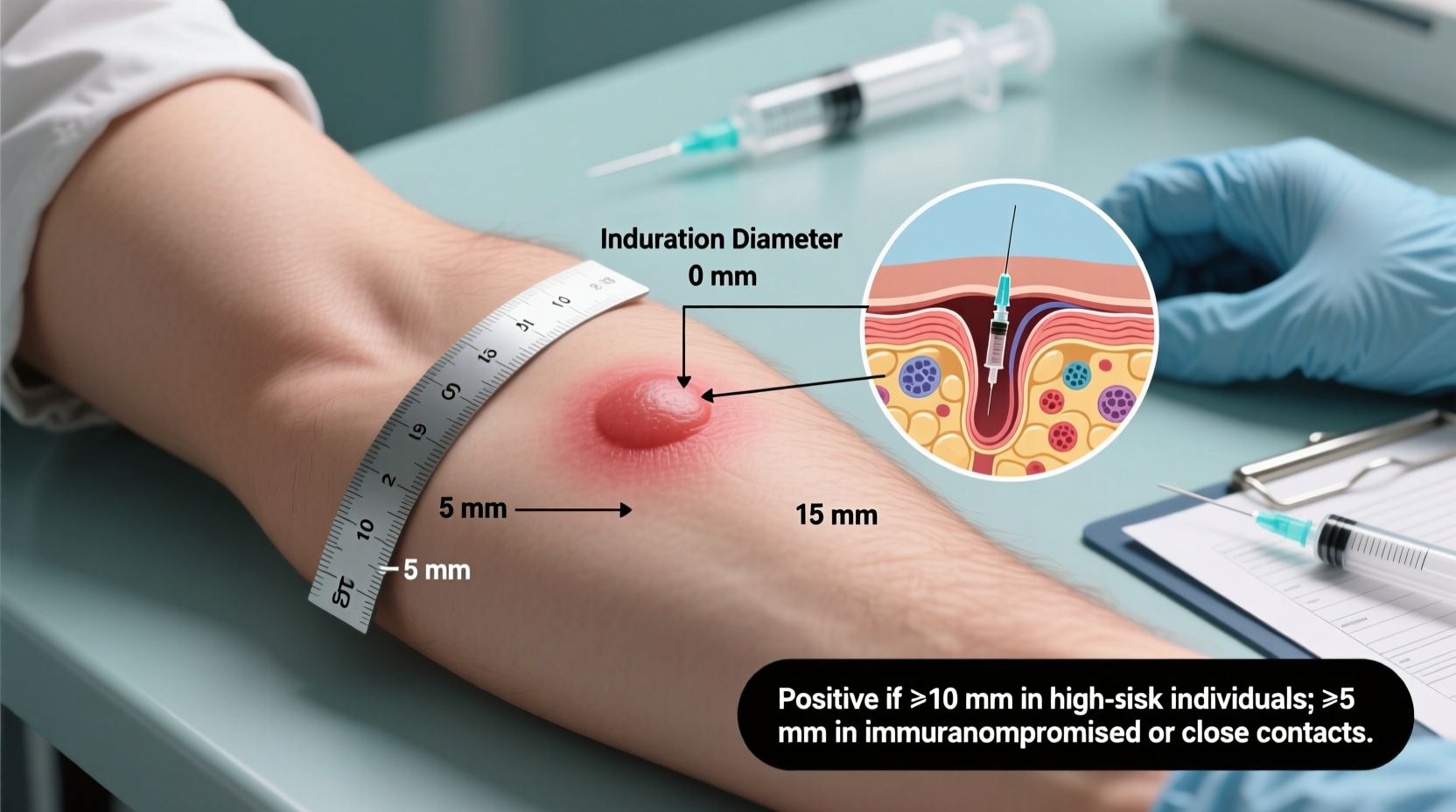
It’s crucial to distinguish between erythema (redness) and induration (a raised, hardened area). Only induration is measured. Redness may be present but does not contribute to the diagnostic interpretation. The size of the induration determines whether the result is considered positive, based on specific risk-based thresholds established by public health authorities like the Centers for Disease Control and Prevention (CDC).
Step-by-Step Guide to Reading the PPD Test
Accurate reading requires a systematic approach. Follow these steps precisely to ensure reliability:
- Schedule the reading: Confirm the patient returns 48–72 hours post-injection. Earlier or later readings reduce validity.
- Locate the injection site: Ask the patient where discomfort or swelling was noted, then visually inspect the forearm.
- P palpate, don’t just look: Use your fingertips to gently feel for firmness. Induration often extends beyond visible changes.
- Measure the induration: Use a transparent ruler to measure the diameter of the hardened area across the forearm (perpendicular to the long axis), in millimeters.
- Record the exact measurement: Document the size numerically—do not round up or categorize prematurely.
- Interpret based on risk factors: Apply CDC guidelines to determine positivity based on the patient’s medical history and exposure risks.
Interpreting Results: Thresholds and Risk Categories
A positive PPD result depends not only on the size of the induration but also on the individual’s risk profile. The CDC defines three primary cutoff levels:
| Risk Category | Induration Size (mm) | Interpretation |
|---|---|---|
| HIV-positive, recent TB contact, fibrotic lung changes | ≥5 mm | Positive |
| Recent immigrants from high-TB-burden countries, IV drug users, residents of congregate settings | ≥10 mm | Positive |
| No known risk factors | ≥15 mm | Positive |
This tiered system ensures that individuals at higher risk are not overlooked due to conservative thresholds. For example, a 6 mm reaction in someone living with HIV should be treated as positive and evaluated further, even though it would be negative in a low-risk person.
“Interpreting a PPD isn't about hitting a single number—it's about understanding the patient’s context. A 10 mm reaction means something very different in a nursing home resident versus a healthy college student.” — Dr. Linda Chen, Infectious Disease Specialist, Johns Hopkins Medicine
Common Errors and How to Avoid Them
Misinterpretation of the PPD test is more common than many realize. Some frequent mistakes include:
- Measuring erythema instead of induration
- Reading the test too early (before 48 hours) or too late (after 72 hours)
- Using improper injection techniques that affect antigen delivery
- Allowing untrained personnel to administer or read the test
- Ignoring patient history when interpreting results
One major pitfall is the \"booster phenomenon,\" particularly relevant in older adults or those previously tested. If a patient has an initially negative result but is retested weeks later and shows a positive response, it may reflect immune recall rather than new infection. This can complicate serial testing programs, such as those in healthcare workers.
Mini Case Study: Missed Diagnosis Due to Improper Reading
A 32-year-old nurse presented for routine employment screening. She received a PPD test during her orientation. The clinic staff member read the test at 76 hours and reported no induration because there was minimal redness. However, the nurse developed a persistent cough six months later and was eventually diagnosed with active pulmonary TB.
Upon review, it was discovered that the initial reader had not palpated the site and failed to notice a 12 mm area of firmness. Because she worked in a high-risk environment (hospital emergency department), even 10 mm should have been considered positive. This oversight delayed preventive therapy and increased her risk of progression to active disease.
This case underscores the importance of proper training and adherence to protocol—not just in administration, but in careful physical examination of the test site.
Checklist for Accurate PPD Interpretation
To ensure consistency and precision, follow this checklist every time you read a PPD test:
- ☑ Confirm the test was administered intradermally with formation of a bleb
- ☑ Verify the time elapsed since injection is between 48 and 72 hours
- ☑ Palpate the site with fingertips to detect induration
- ☑ Measure the transverse diameter of induration in millimeters
- ☑ Ignore erythema; record only firm swelling
- ☑ Assess patient-specific risk factors before labeling result
- ☑ Document findings clearly in the medical record
- ☑ Refer positive cases for chest X-ray and clinical evaluation
Frequently Asked Questions
Can medications affect PPD test results?
Yes. Immunosuppressive drugs such as corticosteroids, TNF-alpha inhibitors (e.g., infliximab), and chemotherapy can suppress the immune response, leading to false-negative results. Patients on these therapies may require alternative testing methods like interferon-gamma release assays (IGRAs).
What should I do if the patient doesn’t return within 72 hours?
If the reading window is missed, the test should be repeated. However, in some occupational or outbreak settings, a second test can be placed immediately without a waiting period. Consult local health department guidelines for specific protocols.
Is the PPD test still reliable given newer blood tests?
The PPD test remains a valuable tool, especially in resource-limited settings. While IGRA blood tests offer advantages like no need for return visits and fewer cross-reactions with BCG vaccine, PPD is cost-effective and widely available. The choice depends on clinical context, availability, and patient factors.
Final Thoughts and Call to Action
Reliable TB screening starts with accurate PPD interpretation. It’s not merely a technical task—it’s a critical step in preventing transmission and protecting vulnerable populations. Whether you're a clinician, nurse, or public health worker, mastering this skill enhances patient outcomes and strengthens community health efforts.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?