Physical activity is essential for long-term health, but for some, it comes with an unwelcome side effect: headaches. If you've ever finished a run, weight session, or intense cardio workout only to be hit by a throbbing pain in your head, you're not alone. Exercise-induced headaches are more common than many realize, yet they're often misunderstood. While dehydration is frequently blamed, exertion itself can also play a significant role. Understanding the difference—and overlap—between these two causes is crucial for prevention and long-term comfort during workouts.
These headaches aren't just inconvenient; they can disrupt fitness routines and reduce motivation. More importantly, mistaking one cause for another may lead to ineffective solutions. For example, drinking more water won’t help if the root issue is vascular strain from intense effort. Conversely, pacing yourself won’t fix a headache caused by chronic underhydration. This article breaks down the physiological mechanisms behind post-exercise headaches, compares dehydration versus exertion as primary triggers, and offers science-backed strategies to keep them at bay.
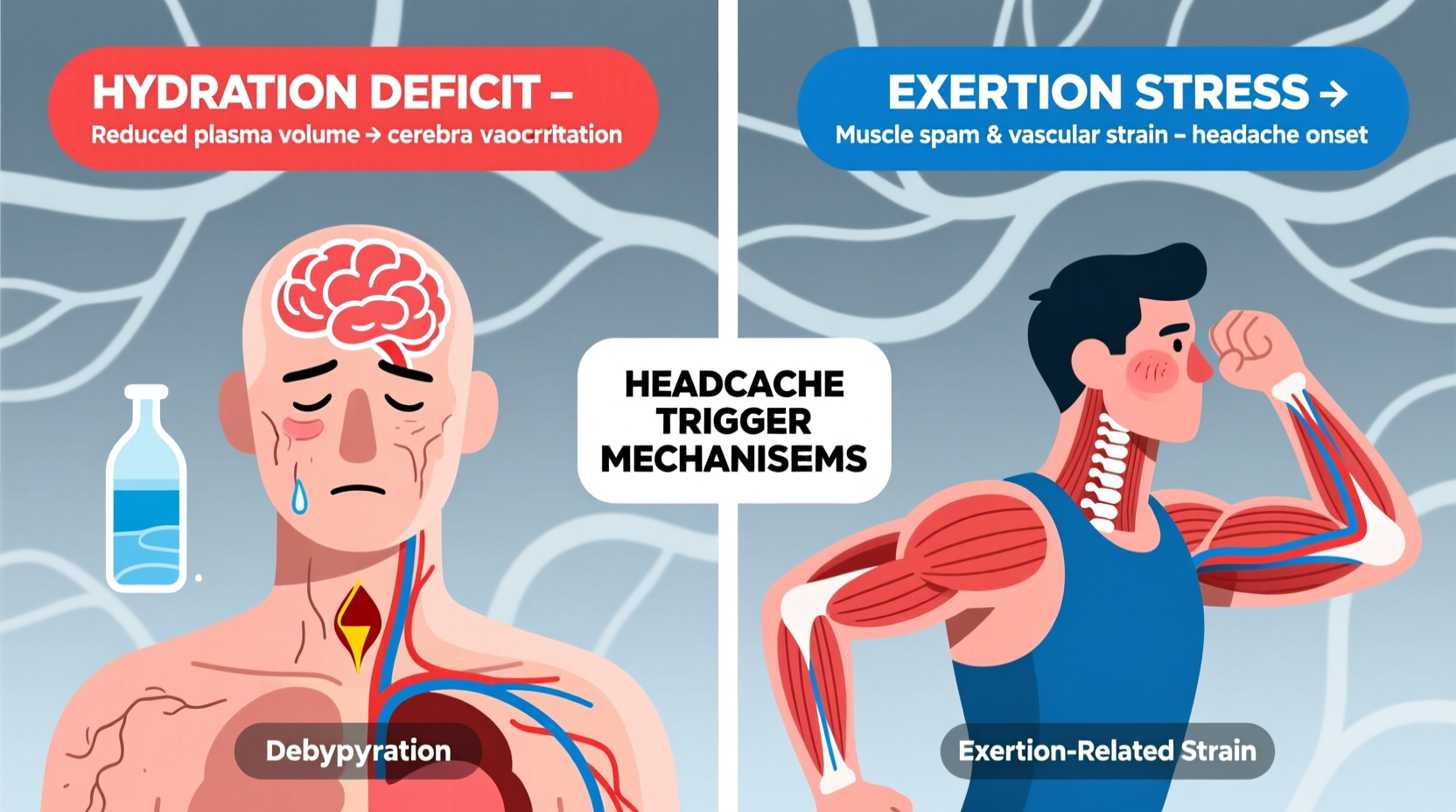
Understanding Exercise-Induced Headaches
Exercise-induced headaches fall into two main categories: primary and secondary. Primary exercise headaches are benign, typically triggered by physical exertion without underlying pathology. These usually present as pulsating pain affecting both sides of the head, lasting from 5 minutes to 48 hours. Secondary exercise headaches stem from structural issues like arterial dissection, tumors, or cerebrospinal fluid leaks, and require medical evaluation.
The focus here is on primary exercise headaches, which are commonly linked to either dehydration or the mechanical and vascular effects of exertion. Both factors can independently cause headaches, but they often coexist, making diagnosis tricky. The key lies in identifying patterns: when the headache occurs, its intensity, duration, and associated symptoms such as dizziness, nausea, or visual disturbances.
Dehydration: The Silent Trigger
Dehydration remains one of the most overlooked yet preventable causes of post-exercise headaches. When fluid loss through sweat exceeds intake, blood volume decreases, reducing oxygen flow to the brain. This hypoperfusion can activate pain-sensitive structures around cerebral vessels, leading to a dull, persistent ache.
Sweat rates vary widely based on intensity, climate, and individual physiology. A 70kg person can lose over 1 liter of fluid per hour during vigorous exercise in hot environments. Even mild dehydration—defined as a 1–2% loss of body weight in fluids—can impair thermoregulation and trigger headaches.
Electrolyte imbalance compounds the problem. Sodium, potassium, and magnesium are lost in sweat, and their depletion affects nerve signaling and vascular tone. Low sodium (hyponatremia), though less common, can also cause severe neurological symptoms, including headache and confusion.
“Even modest dehydration can alter brain function and increase headache susceptibility. Athletes often underestimate their fluid needs until symptoms appear.” — Dr. Lena Patel, Sports Medicine Specialist
Signs You Might Be Dehydrated During Exercise
- Dark yellow urine or reduced urination frequency
- Dry mouth and thirst
- Fatigue or lightheadedness
- Muscle cramps
- Headache that improves with rehydration
Exertion: The Physical Stress Factor
Unlike dehydration-related headaches, exertional headaches arise directly from the physiological demands of intense activity. These are thought to result from increased intracranial pressure and dilation of blood vessels in the brain during strenuous efforts. Activities involving heavy lifting, sprinting, or prolonged high-intensity intervals are particularly prone to triggering this response.
The mechanism involves sudden rises in blood pressure and cardiac output. As heart rate spikes, cerebral blood flow increases rapidly. In susceptible individuals, this surge can stretch pain-sensitive arteries, causing a bilateral, pulsating headache. These headaches typically begin during or immediately after peak exertion and may last longer than dehydration-related ones.
Genetic predisposition plays a role. People with a history of migraines or vascular sensitivity are more likely to experience exertion-triggered headaches. Additionally, exercising in extreme temperatures—especially heat or high altitude—can amplify vascular stress, increasing risk.
When Exertion Is the Primary Culprit
- Headache begins during maximal effort (e.g., final sprint or heavy lift)
- Pain is throbbing and bilateral, often worsening with continued strain
- No signs of dehydration despite similar conditions in past workouts
- Occurs even with adequate pre-hydration and electrolyte balance
Comparing Dehydration vs. Exertion: Key Differences
| Factor | Dehydration-Related Headache | Exertion-Related Headache |
|---|---|---|
| Onset | Gradual, during or after prolonged activity | Sudden, during peak exertion |
| Pain Type | Dull, constant, front or whole-head | Pulsating, throbbing, bilateral |
| Duration | Minutes to several hours | Several minutes to 48 hours |
| Relief Factors | Rehydration, rest, cooling down | Rest, reduced intensity, NSAIDs |
| Associated Symptoms | Dry mouth, fatigue, dark urine | Nausea, dizziness, flushing |
| Prevention Focus | Fluid and electrolyte intake | Workout pacing, conditioning |
This comparison underscores why accurate self-assessment matters. Misdiagnosing an exertion-based headache as dehydration might lead to excessive fluid intake without addressing the real issue—intensity management.
Real-World Scenario: A Runner’s Experience
Consider Sarah, a 32-year-old recreational runner training for her first half-marathon. She began experiencing headaches after long runs, especially in summer. Initially, she assumed dehydration was the cause and started drinking large amounts of water before and during runs. Yet the headaches persisted.
Upon reviewing her logs, she noticed a pattern: headaches occurred primarily during tempo runs or hill repeats—not during steady-state jogs—even when hydration was consistent. She also experienced brief dizziness and facial flushing at the peak of exertion.
After consulting a sports physician, Sarah learned she was likely suffering from exertional headaches exacerbated by heat. Her solution wasn’t more water, but adjusting her pacing strategy, incorporating walk breaks during intense segments, and using cooling techniques like pouring water over her head. Within weeks, her headaches subsided.
Sarah’s case illustrates how easily exertion can be masked as dehydration—especially when both factors are present. The critical insight came from tracking context, not just symptoms.
Effective Prevention Strategies
Preventing post-exercise headaches requires a dual approach: optimizing hydration and managing exertion intelligently. One doesn’t replace the other; both are foundational.
Hydration Best Practices
- Drink 16–20 oz (500–600 ml) of water 2–3 hours before exercise
- Consume 7–10 oz (200–300 ml) every 10–20 minutes during activity
- Rehydrate with electrolyte-enhanced fluids after prolonged or intense sessions
- Weigh yourself before and after workouts; drink 16–24 oz per pound lost
Exertion Management Techniques
- Warm up properly: 10–15 minutes of light aerobic activity prepares cardiovascular system
- Avoid sudden surges in intensity; use perceived exertion scales (e.g., RPE 6–8/10) to stay in safe zones
- Break intense workouts into intervals with recovery periods
- Strengthen neck and core muscles to improve posture and reduce vascular strain
- Cool down gradually to allow blood pressure to normalize
When to Seek Medical Advice
While most exercise-related headaches are benign, certain red flags warrant immediate medical attention:
- Sudden, \"thunderclap\" headache at onset
- Headache accompanied by vomiting, confusion, or vision changes
- Neck stiffness or fever
- Loss of consciousness or numbness
- First occurrence after age 40 or with no prior history
These could indicate secondary causes such as subarachnoid hemorrhage, cervical artery dissection, or idiopathic intracranial hypertension. Imaging studies like MRI or CT scans may be necessary to rule out serious conditions.
FAQ: Common Questions About Post-Exercise Headaches
Can caffeine help prevent exercise-induced headaches?
Caffeine can constrict blood vessels and may reduce headache severity in some people. However, regular users may experience rebound headaches if they skip their usual dose. Moderate intake (e.g., a small coffee 30–60 minutes before exercise) may help, but dependency should be avoided.
Are certain types of exercise more likely to cause headaches?
Yes. Activities involving straining—such as weightlifting, rowing, or sprinting—are higher risk due to rapid blood pressure spikes. Yoga inversions (like headstands) can also trigger headaches in sensitive individuals. Low-impact exercises like walking, cycling, or swimming pose lower risk when performed at moderate intensity.
Is it safe to continue exercising if I get frequent post-workout headaches?
If headaches are mild, predictable, and resolve quickly with rest, adjustments to hydration and pacing may suffice. However, frequent or worsening headaches should prompt evaluation by a healthcare provider to rule out underlying conditions.
Step-by-Step Action Plan
- Track Symptoms: Keep a log of workouts, hydration, environment, and headache occurrence for two weeks.
- Optimize Hydration: Follow pre-, during, and post-exercise fluid guidelines. Include electrolytes for sessions over 60 minutes.
- Modify Intensity: Reduce peak effort temporarily and use interval training to build tolerance.
- Improve Warm-Up/Cool-Down: Dedicate 10 minutes to each phase to stabilize cardiovascular response.
- Consult a Professional: If headaches persist, see a sports medicine doctor or neurologist for assessment.
Conclusion: Take Control of Your Workouts
Headaches after exercise don’t have to be inevitable. Whether driven by dehydration, exertion, or a combination of both, these discomforts are manageable with informed strategies. Recognizing the nuances between causes empowers you to make precise adjustments—drinking smarter, pacing better, and training safer.
Your body sends signals for a reason. Listening carefully, responding proactively, and seeking expert input when needed transforms setbacks into opportunities for improvement. Don’t let post-workout headaches derail your progress. Apply these insights today, refine your routine, and reclaim the joy of movement—pain-free.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?