Suddenly feeling lightheaded or unsteady after rising from a seated or lying position is a surprisingly common experience. You stand up quickly, and for a few seconds, the room seems to tilt or your vision blurs. While usually brief and harmless, this sensation can be disorienting—and sometimes dangerous if it leads to a fall. Known medically as orthostatic hypotension or postural hypotension, this dizziness occurs due to a rapid drop in blood pressure when changing positions. Understanding the mechanisms behind this response, identifying contributing factors, and adopting preventive measures can help you maintain balance and avoid unnecessary risks.
The Science Behind Postural Dizziness
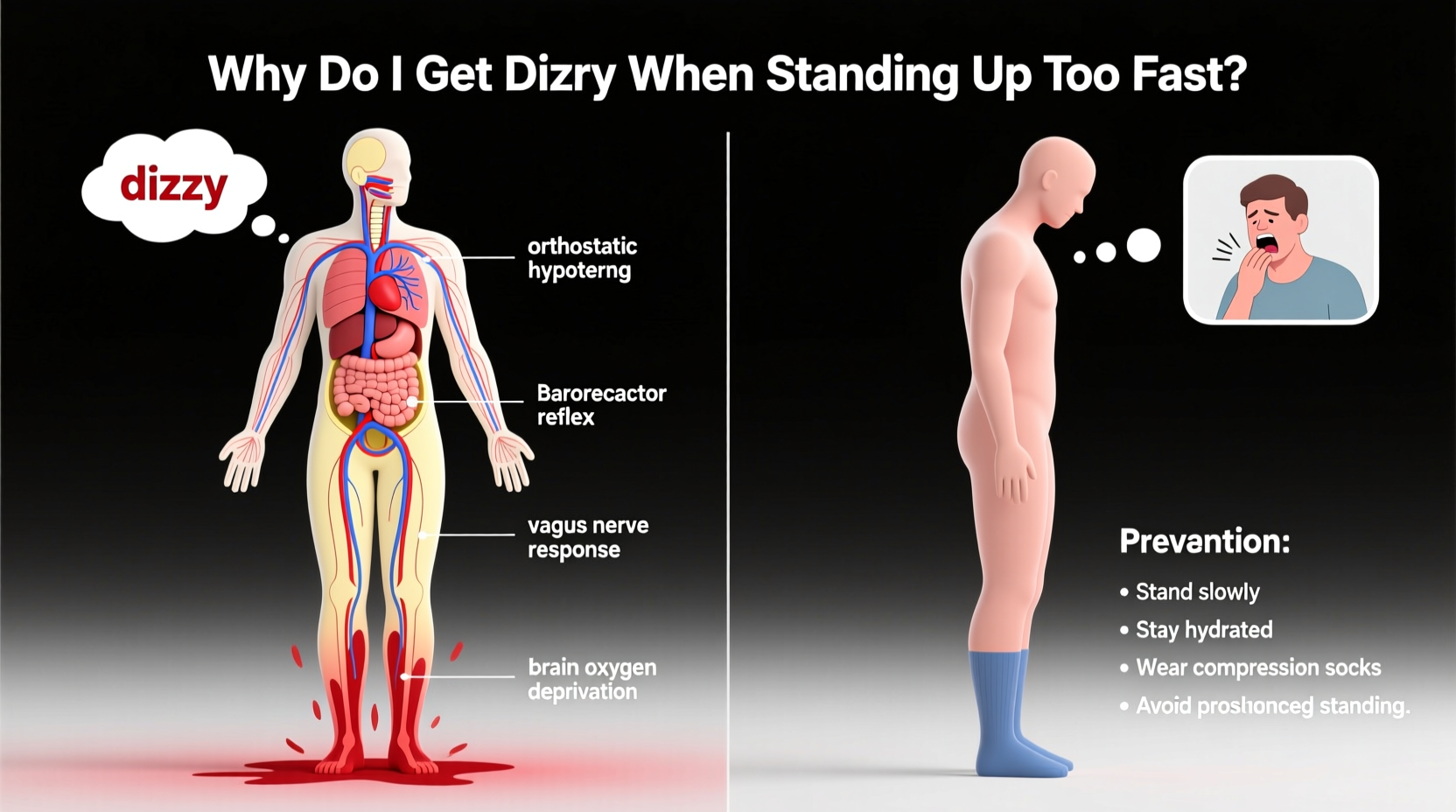
When you lie down, your heart doesn’t have to work hard to circulate blood—gravity affects blood distribution evenly. But when you stand up, gravity pulls blood downward into your legs and abdomen. This sudden shift reduces the amount of blood returning to your heart, which in turn lowers cardiac output and blood pressure. Normally, your autonomic nervous system compensates within seconds by constricting blood vessels and increasing heart rate to maintain adequate blood flow to the brain.
However, if this reflex is delayed or impaired, even briefly, blood pressure drops faster than the body can correct it. The result? Reduced oxygen supply to the brain causes transient symptoms like dizziness, lightheadedness, blurred vision, or even fainting. This condition is called orthostatic hypotension, defined as a drop of at least 20 mm Hg in systolic blood pressure or 10 mm Hg in diastolic pressure within three minutes of standing.
“Orthostatic hypotension is one of the most common forms of low blood pressure, especially among older adults. It’s often overlooked but can significantly impact quality of life and increase fall risk.” — Dr. Rebecca Langston, Neurologist and Autonomic Specialist
Common Causes of Standing-Induced Dizziness
While occasional dizziness upon standing may happen to anyone, frequent or severe episodes suggest underlying causes. These range from mild dehydration to chronic medical conditions. Recognizing the root cause is essential for effective management.
Dehydration
Insufficient fluid intake reduces blood volume, making it harder for the body to maintain pressure when upright. Dehydration is especially common in hot weather, during illness, or after intense physical activity without proper rehydration.
Medications
Many prescription drugs affect blood pressure regulation. Common culprits include:
- Diuretics (water pills)
- Blood pressure medications (beta-blockers, ACE inhibitors)
- Antidepressants (especially tricyclics)
- Parkinson’s disease treatments
- Some erectile dysfunction drugs
Aging and Nervous System Changes
As we age, the autonomic nervous system becomes less responsive. Blood vessel elasticity decreases, and baroreceptor sensitivity—the sensors that detect blood pressure changes—declines. This makes older adults more prone to postural drops in blood pressure, particularly those over 65.
Medical Conditions
Certain health issues disrupt normal blood pressure control:
- Diabetes: Can damage nerves involved in blood pressure regulation (autonomic neuropathy).
- Parkinson’s disease: Affects autonomic function and dopamine-related vascular control.
- Heart problems: Arrhythmias, heart failure, or valve disorders reduce cardiac efficiency.
- Anemia: Low red blood cell count impairs oxygen delivery, worsening dizziness.
- Adrenal insufficiency: Conditions like Addison’s disease impair hormone regulation of blood pressure.
Diet and Lifestyle Factors
Skipping meals, consuming large carbohydrate-rich meals, or drinking alcohol can all contribute. Large meals divert blood to the digestive tract, reducing availability for the brain. Alcohol dilates blood vessels and dehydrates the body, amplifying the risk.
Prevention Strategies to Reduce Dizziness
Most cases of orthostatic dizziness are manageable with lifestyle adjustments. Implementing consistent habits can dramatically reduce episodes and improve stability.
Stay Hydrated
Maintaining adequate fluid intake helps sustain blood volume. Aim for 6–8 glasses of water daily, more in warm climates or during exercise. Some individuals benefit from slightly increasing salt intake under medical supervision, as sodium helps retain fluid and boost blood pressure.
Rise Slowly
Give your body time to adjust. Instead of jumping out of bed, follow this sequence:
- Wake up and remain lying for 30 seconds.
- Sit on the edge of the bed for another 30 seconds.
- Stand up slowly and pause for a moment before walking.
Compression Stockings
These garments apply gentle pressure to the legs, preventing blood from pooling. They’re especially useful for people with chronic venous insufficiency or those who stand for long periods.
Exercise Regularly
Cardiovascular fitness strengthens the heart and improves circulation. Activities like walking, swimming, or cycling enhance vascular tone and autonomic responsiveness over time.
Review Medications with Your Doctor
If you're on medication and experiencing frequent dizziness, don't stop taking it—but do discuss it with your physician. Adjustments in dosage, timing, or alternative prescriptions may resolve the issue.
| Do’s | Don’ts |
|---|---|
| Drink water throughout the day | Go for hours without fluids |
| Move gradually from lying to standing | Jump up quickly after resting |
| Eat smaller, balanced meals | Consume large, carb-heavy meals |
| Wear compression socks if recommended | Stand still for long periods |
| Monitor symptoms and report changes | Ignore recurrent dizziness or near-fainting |
Real-Life Scenario: Managing Morning Dizziness
Consider Maria, a 72-year-old retired teacher who began experiencing frequent dizziness upon waking. She’d often grab the wall to steady herself and once fell while trying to reach the bathroom. Concerned, she visited her primary care doctor. Her blood pressure was normal while sitting but dropped sharply when standing. Further evaluation revealed mild dehydration, long-term use of a diuretic for hypertension, and reduced mobility due to knee pain limiting her exercise.
Her doctor adjusted her medication timing to earlier in the day, advised increased fluid and electrolyte intake, and prescribed thigh-high compression stockings. Maria also started a gentle morning routine: stretching in bed before sitting up slowly and pausing before standing. Within two weeks, her symptoms improved significantly. She regained confidence and reduced her fall risk through simple, targeted changes.
“Maria’s case shows how multiple small factors—medication, hydration, movement habits—can combine to cause dizziness. Addressing each one systematically led to meaningful improvement.” — Dr. Alan Zhou, Internal Medicine Physician
Step-by-Step Guide to Safer Position Changes
For those prone to dizziness, adopting a structured transition routine can prevent sudden drops in blood pressure. Follow these steps each time you rise from bed or a seated position:
- Pause and Breathe: Before moving, take three deep breaths to prepare your cardiovascular system.
- Lie to Sit: Roll to your side, then push yourself up to a seated position on the edge of the bed or chair. Keep feet flat on the floor.
- Wait 30 Seconds: Allow your body to adjust. Avoid rushing this phase.
- Check for Symptoms: If you feel lightheaded, wait longer until the sensation passes.
- Stand Slowly: Use support (like a handrail or armrest) to rise. Stand still for 10–15 seconds before walking.
- Move Cautiously: Take slow, deliberate steps, especially in dim lighting or unfamiliar environments.
Frequently Asked Questions
Is it normal to feel dizzy every time I stand up?
No. Occasional mild dizziness may happen, but frequent or severe episodes are not normal and should be evaluated. Recurrent symptoms could indicate an underlying condition such as autonomic dysfunction, dehydration, or medication side effects.
Can low iron cause dizziness when standing?
Yes. Iron deficiency anemia reduces the blood’s oxygen-carrying capacity. When combined with positional changes, this can lead to pronounced dizziness, fatigue, and shortness of breath. A simple blood test can confirm iron levels.
Should I worry if I almost faint when standing?
Yes. Near-fainting (presyncope) or actual fainting (syncope) upon standing increases fall risk and may signal serious cardiovascular or neurological issues. Seek medical evaluation, especially if episodes occur regularly or are accompanied by chest pain, palpitations, or confusion.
Conclusion: Take Control of Your Stability
Dizziness when standing up too fast is more than just a minor inconvenience—it’s a signal from your body that something in your circulatory or nervous system needs attention. While often benign, untreated orthostatic hypotension can compromise independence, especially in older adults. The good news is that most cases respond well to hydration, gradual movement, medication review, and lifestyle improvements.
You don’t have to live with constant lightheadedness. By understanding the causes and applying practical prevention strategies, you can move through your day with greater confidence and safety. Start today: hydrate, slow down your transitions, and talk to your healthcare provider if symptoms persist. Small changes now can lead to lasting improvements in how you feel and function.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?