Under-the-skin pimples—often referred to as blind pimples or closed comedones—are a common yet frustrating form of acne. Unlike surface-level whiteheads or blackheads, these bumps develop deep beneath the skin’s surface, causing redness, swelling, and tenderness without a visible head. They can linger for days or even weeks, resisting typical spot treatments. Understanding what causes them and how to treat them effectively is essential for anyone struggling with persistent breakouts.
What Are Under-the-Skin Pimples?
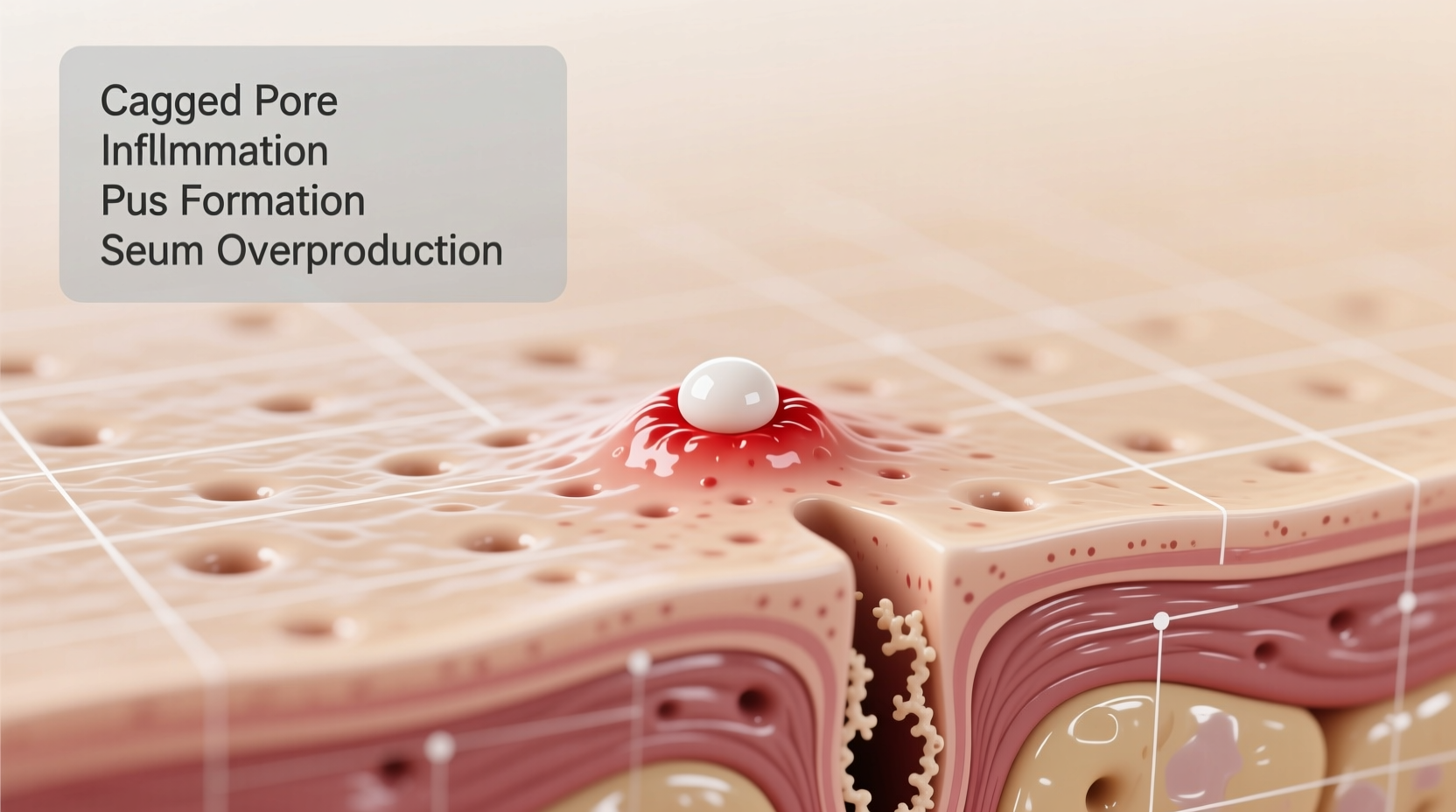
Under-the-skin pimples are inflamed lesions that form when hair follicles become clogged with oil (sebum), dead skin cells, and bacteria. Because they don’t reach the surface, they lack the white or black tip seen in other acne types. Instead, they manifest as firm, painful lumps beneath the skin, most commonly on the forehead, chin, jawline, and cheeks.
Medically, these are often classified as nodules or cysts when severe. Nodules are hard, deeply embedded inflammations, while cysts are softer, pus-filled sacs. Both require targeted care to avoid scarring and prolonged healing times.
Common Causes of Blind Pimples
The development of under-the-skin pimples is rarely due to a single factor. It’s usually a combination of biological, environmental, and lifestyle influences. Here are the primary causes:
- Excess sebum production: Overactive sebaceous glands produce too much oil, which mixes with dead skin cells and blocks pores.
- Hormonal fluctuations: Androgens rise during puberty, menstruation, pregnancy, or conditions like PCOS, stimulating oil production and triggering acne.
- Bacterial buildup: Cutibacterium acnes (formerly P. acnes) thrives in clogged follicles, causing inflammation and swelling.
- Dead skin cell accumulation: Poor exfoliation leads to a buildup that traps oil and bacteria below the surface.
- Dietary triggers: High-glycemic foods (like sugar and refined carbs) and dairy have been linked to increased acne severity in some individuals.
- Stress: Elevated cortisol levels can stimulate oil glands and weaken the skin’s barrier function.
- Skincare product misuse: Heavy moisturizers, comedogenic makeup, or over-cleansing can disrupt the skin’s balance and clog pores.
“Blind pimples often result from deep follicular inflammation before it reaches the surface. Early intervention with anti-inflammatory ingredients can reduce progression.” — Dr. Lena Torres, Board-Certified Dermatologist
Effective Treatment Options
Treating under-the-skin pimples requires patience and consistency. Since they’re rooted deep in the dermis, topical solutions alone may not suffice. A layered approach works best.
Topical Treatments
These help regulate oil, exfoliate, and reduce bacterial growth:
- Salicylic acid: A beta-hydroxy acid (BHA) that penetrates oil to exfoliate inside the pore.
- Benzoyl peroxide: Kills acne-causing bacteria and reduces inflammation.
- Niacinamide: Calms redness and strengthens the skin barrier.
- Retinoids (e.g., adapalene): Promote cell turnover and prevent clogging.
Professional Treatments
For stubborn or recurring cases, dermatological interventions offer faster results:
- Corticosteroid injections: Reduce swelling and flatten nodules within 24–48 hours.
- Drainage and extraction: Performed by a professional to safely remove contents without scarring.
- Oral medications: Antibiotics, birth control pills (for hormonal acne), or isotretinoin (Accutane) for severe cystic acne.
At-Home Care Strategies
Support healing and prevent future breakouts with consistent routines:
- Wash your face twice daily with a gentle, non-comedogenic cleanser.
- Apply a salicylic acid toner or serum to problem areas nightly.
- Use a warm compress to encourage blood flow and gradual release of trapped debris.
- Maintain hydration with a lightweight, oil-free moisturizer.
- Avoid touching your face or resting phones/headphones against your skin.
| Treatment Type | Best For | Time to See Results |
|---|---|---|
| Salicylic Acid | Mild to moderate clogged pores | 2–4 weeks |
| Benzoyl Peroxide | Inflammatory, bacteria-driven acne | 1–3 weeks |
| Adapalene Gel | Preventing new breakouts | 3–6 weeks |
| Cortisone Injection | Large, painful nodules | 24–72 hours |
| Oral Antibiotics | Moderate to severe inflammatory acne | 4–6 weeks |
Prevention Checklist
Preventing under-the-skin pimples involves addressing root causes before they escalate. Follow this actionable checklist to minimize flare-ups:
- ✅ Cleanse your face morning and night with a pH-balanced cleanser.
- ✅ Exfoliate 2–3 times weekly using a BHA (salicylic acid).
- ✅ Avoid heavy, oil-based makeup and skincare products.
- ✅ Change pillowcases every 3–4 days to reduce bacterial transfer.
- ✅ Manage stress through sleep, exercise, or mindfulness practices.
- ✅ Limit high-glycemic foods and monitor dairy intake if breakouts persist.
- ✅ Consult a dermatologist if acne affects self-esteem or leaves scars.
Real-Life Example: Managing Hormonal Breakouts
Sophia, a 28-year-old graphic designer, struggled with recurring under-the-skin pimples along her jawline every month before her period. Despite trying various spot treatments, the bumps would return with the same intensity. After tracking her cycle and consulting a dermatologist, she learned her acne was hormonally driven.
Her doctor recommended a combination of topical adapalene at night, a salicylic acid wash in the morning, and a low-dose oral contraceptive to regulate androgen levels. Within three months, her premenstrual breakouts decreased significantly. She also adopted a routine of changing her phone screen wipe weekly and managing stress with yoga, further improving her skin clarity.
This case highlights how identifying the underlying cause—especially hormonal imbalance—is crucial for long-term improvement.
Frequently Asked Questions
Can drinking more water clear under-the-skin pimples?
While staying hydrated supports overall skin health, drinking water alone won’t eliminate blind pimples. Acne is primarily driven by hormones, bacteria, and clogged pores. Hydration helps maintain the skin barrier but must be paired with proper cleansing and treatment for visible results.
Why do I only get these pimples on my chin and jawline?
This pattern is often linked to hormonal acne. The lower face contains a higher concentration of oil glands influenced by androgens. Fluctuations during menstrual cycles, stress, or endocrine disorders like PCOS frequently trigger breakouts in this zone.
Is it safe to use acne patches on blind pimples?
Traditional hydrocolloid patches work best on open wounds or whiteheads. However, patches infused with salicylic acid or tea tree oil can help deliver active ingredients to under-the-skin pimples. Look for medicated versions designed for pre-pimple stages.
Conclusion: Take Control of Your Skin Health
Under-the-skin pimples are more than just a cosmetic concern—they signal deeper imbalances in your skin and body. By understanding the causes, adopting targeted treatments, and maintaining preventive habits, you can reduce their frequency and severity. Consistency is key. What works for one person may not work for another, so track your routine and adjust based on results.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?