Bruises are a common part of life—most people experience them after minor bumps or knocks. But while some individuals might only show a faint mark from a significant impact, others develop large, discolored patches from barely noticeable contact. This variation isn't random. The tendency to bruise easily is influenced by a complex interplay of biological, environmental, and health-related factors. Understanding why some people bruise more readily than others can help identify whether it’s a normal variation or a sign of an underlying condition.
The Science Behind Bruising
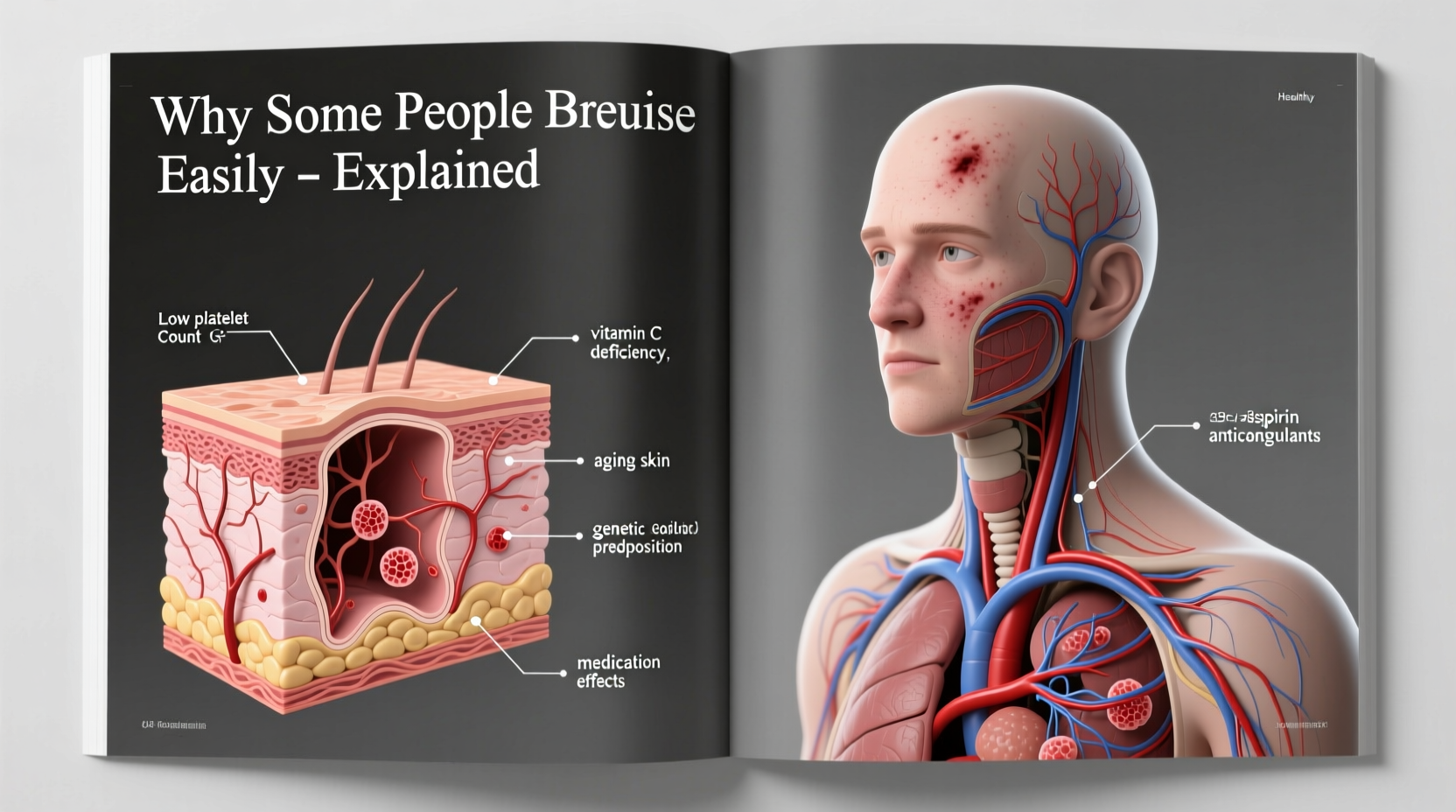
A bruise, medically known as a hematoma or contusion, occurs when small blood vessels under the skin—called capillaries—break due to trauma. Blood leaks into surrounding tissues, causing the characteristic blue, purple, or yellow discoloration. Over time, the body reabsorbs this blood, and the bruise fades through various color stages before disappearing.
The speed and severity of bruising depend on several physiological processes:
- Vessel fragility: How easily capillaries rupture under pressure.
- Skin thickness and elasticity: Thinner or less elastic skin offers less protection to blood vessels.
- Platelet function: Platelets are blood cells that initiate clotting to stop bleeding.
- Coagulation factors: Proteins in the blood that work with platelets to form clots.
When any of these components are compromised, even mild pressure can cause visible bruising.
Genetic and Biological Factors
Some people are simply born with bodies that are more prone to bruising. Genetics play a foundational role in determining skin structure, vessel strength, and clotting efficiency.
For example, individuals with fair or thin skin—often seen in those with lighter complexions—are more likely to show bruises. Their dermal layer provides less cushioning for capillaries, making them more vulnerable to damage. Similarly, collagen production, which maintains skin integrity, varies genetically. Lower natural collagen levels mean weaker vessel support.
Women tend to bruise more easily than men, partly due to differences in subcutaneous fat distribution and hormonal influences. Estrogen affects capillary wall stability, and fluctuations during menstrual cycles or hormone therapy can increase susceptibility.
“Some patients come in alarmed by frequent bruising, only to learn it’s been a lifelong trait with no underlying disease. Family history often holds clues.” — Dr. Alan Reeves, Hematologist at Boston General Hospital
Age-Related Changes in Skin and Vessels
One of the most well-documented reasons for increased bruising is aging. As people grow older, their skin undergoes several changes that make bruising more common:
- Thinning of the epidermis and dermis: The skin becomes less dense and loses protective fat layers.
- Decreased collagen and elastin: These proteins keep skin firm and resilient; their decline leads to fragile capillaries.
- Weakened blood vessel walls: Aging capillaries are more prone to rupture under minimal stress.
This combination creates what doctors call “senile purpura” or “actinic purpura”—a condition where minor trauma results in large, persistent bruises, typically on the backs of hands and forearms. While not dangerous in itself, it signals increased skin vulnerability.
Chronic sun exposure accelerates these changes. UV radiation damages connective tissue and weakens blood vessel support structures, compounding age-related fragility.
Medical Conditions That Increase Bruising
Frequent or unexplained bruising can sometimes indicate an underlying health issue. Several medical conditions affect the body’s ability to maintain vascular integrity or control bleeding.
Blood Disorders
Conditions affecting platelets or clotting factors can lead to excessive bruising:
- Thrombocytopenia: Low platelet count reduces the blood’s ability to clot.
- Hemophilia and von Willebrand disease: Inherited disorders impairing clotting factor activity.
- Leukemia: Cancer of the blood-forming tissues can disrupt normal platelet production.
Autoimmune Diseases
Some autoimmune conditions attack platelets or blood vessels directly:
- Idiopathic thrombocytopenic purpura (ITP): Immune system destroys platelets.
- Systemic lupus erythematosus (SLE): Can cause vasculitis (inflamed blood vessels) and low platelets.
Liver Disease
The liver produces many clotting factors. Chronic liver conditions like cirrhosis reduce their synthesis, increasing bleeding risk and bruising.
Vitamin Deficiencies
Nutritional deficits also contribute:
- Vitamin C deficiency (scurvy): Weakens blood vessel walls and impairs collagen formation.
- Vitamin K deficiency: Essential for activating clotting proteins; often seen with malabsorption or long-term antibiotic use.
- Vitamin B12 and folate: Necessary for healthy blood cell production.
| Condition | How It Causes Bruising | Common Signs Beyond Bruising |
|---|---|---|
| Thrombocytopenia | Low platelet count impairs clot formation | Petechiae (tiny red dots), nosebleeds, prolonged bleeding |
| Vitamin C Deficiency | Weakens capillary walls and collagen | Fatigue, swollen gums, joint pain |
| Liver Cirrhosis | Reduced production of clotting factors | Jaundice, abdominal swelling, fatigue |
| Senile Purpura | Age-related skin and vessel fragility | Bruises mainly on hands/forearms, no other symptoms |
Medications and Supplements That Promote Bruising
Many commonly used drugs interfere with blood clotting or vessel strength. Even over-the-counter substances can significantly increase bruising risk.
Anticoagulants and Antiplatelets
- Warfarin, heparin: Prescribed to prevent strokes and blood clots.
- Aspirin, clopidogrel: Prevent platelets from clumping together.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
Drugs like ibuprofen and naproxen not only reduce inflammation but also temporarily impair platelet function—even with short-term use.
Corticosteroids
Long-term use of oral or inhaled steroids thins the skin and weakens blood vessels, especially on the arms and face.
Dietary Supplements
Several natural products have blood-thinning effects:
- Fish oil: Contains omega-3 fatty acids that reduce platelet aggregation.
- Ginkgo biloba: Known to inhibit clotting.
- Vitamin E (high doses): Can act as an anticoagulant.
When to Be Concerned: Red Flags for Easy Bruising
Occasional bruising, especially after known injury, is normal. However, certain patterns should prompt medical evaluation:
- Bruises appearing without any identifiable cause
- Large or rapidly spreading bruises from minor contact
- Bruising in unusual locations (back, stomach, face)
- Accompanying symptoms like fatigue, weight loss, or frequent nosebleeds
- Sudden onset of easy bruising in someone who previously didn’t bruise easily
These signs could point to a systemic issue such as a blood disorder, autoimmune disease, or malignancy.
Mini Case Study: Unexplained Bruising Leads to Diagnosis
Sarah, a 52-year-old teacher, began noticing large purple marks on her forearms despite no falls or bumps. Initially dismissing them as age-related, she became concerned when bruises appeared on her torso. Her primary care physician ordered blood tests, which revealed a low platelet count. Further investigation led to a diagnosis of early-stage chronic lymphocytic leukemia (CLL). With timely treatment, Sarah managed the condition effectively. Her case underscores how seemingly minor symptoms like easy bruising can be early indicators of serious illness.
Practical Steps to Reduce Bruising Risk
While some factors like genetics and age can’t be changed, several strategies can help minimize bruising:
- Protect your skin: Wear long sleeves and padding during physical activities.
- Improve lighting at home: Prevent accidental bumps in dim areas.
- Review medications: Ask your doctor if any prescriptions or supplements could be contributing.
- Eat a nutrient-rich diet: Focus on vitamin C (citrus, bell peppers), vitamin K (leafy greens), and bioflavonoids (berries, dark chocolate).
- Stay hydrated: Proper hydration supports skin elasticity and circulation.
Checklist: What to Do If You Bruise Easily
- ✅ Track when and where bruises appear
- ✅ Note any recent medication changes
- ✅ Assess for additional symptoms (fatigue, bleeding gums)
- ✅ Take photos of recurring or unusual bruises
- ✅ Schedule a blood test panel with your doctor if concerned
Frequently Asked Questions
Can dehydration cause bruising?
Dehydration doesn’t directly cause bruising, but it can reduce skin elasticity and impair circulation, making capillaries more vulnerable. Chronically dehydrated skin may heal slower, prolonging the appearance of bruises.
Are children who bruise easily at risk for a bleeding disorder?
Active children often bruise from normal play and usually don’t have underlying issues. However, if bruises are unusually large, occur without trauma, or are accompanied by nosebleeds or gum bleeding, a pediatrician should evaluate for clotting disorders.
Do varicose veins make you bruise more easily?
Yes. Varicose veins involve weakened, dilated blood vessels near the skin surface. These are more prone to rupture, leading to localized bruising, especially in the lower legs.
Conclusion: Understanding Your Body’s Signals
Bruising is more than just a cosmetic concern—it’s a window into your vascular health, nutritional status, and overall well-being. While many cases of easy bruising are harmless and related to age or genetics, persistent or unexplained bruising deserves attention. By understanding the factors at play—from medications to medical conditions—you empower yourself to take proactive steps toward better health.
If you’ve noticed a change in how easily you bruise, don’t ignore it. Keep a simple log, review your medications, and consult a healthcare provider when in doubt. Early detection of underlying conditions can make all the difference. Your body communicates through symptoms—learning to listen can lead to smarter, healthier choices.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?