Bad breath, or halitosis, affects millions of people worldwide—even those who maintain a rigorous oral hygiene routine. You brush twice a day, floss daily, swish with mouthwash, and yet, when you speak closely with someone or check your breath on your hand, the unpleasant odor persists. This can be frustrating, embarrassing, and at times, confusing. The truth is, while brushing, flossing, and rinsing are essential, they don’t address every cause of chronic bad breath. Understanding the deeper reasons behind lingering odor is the first step toward truly fresh breath.
Common Causes Beyond Poor Oral Hygiene
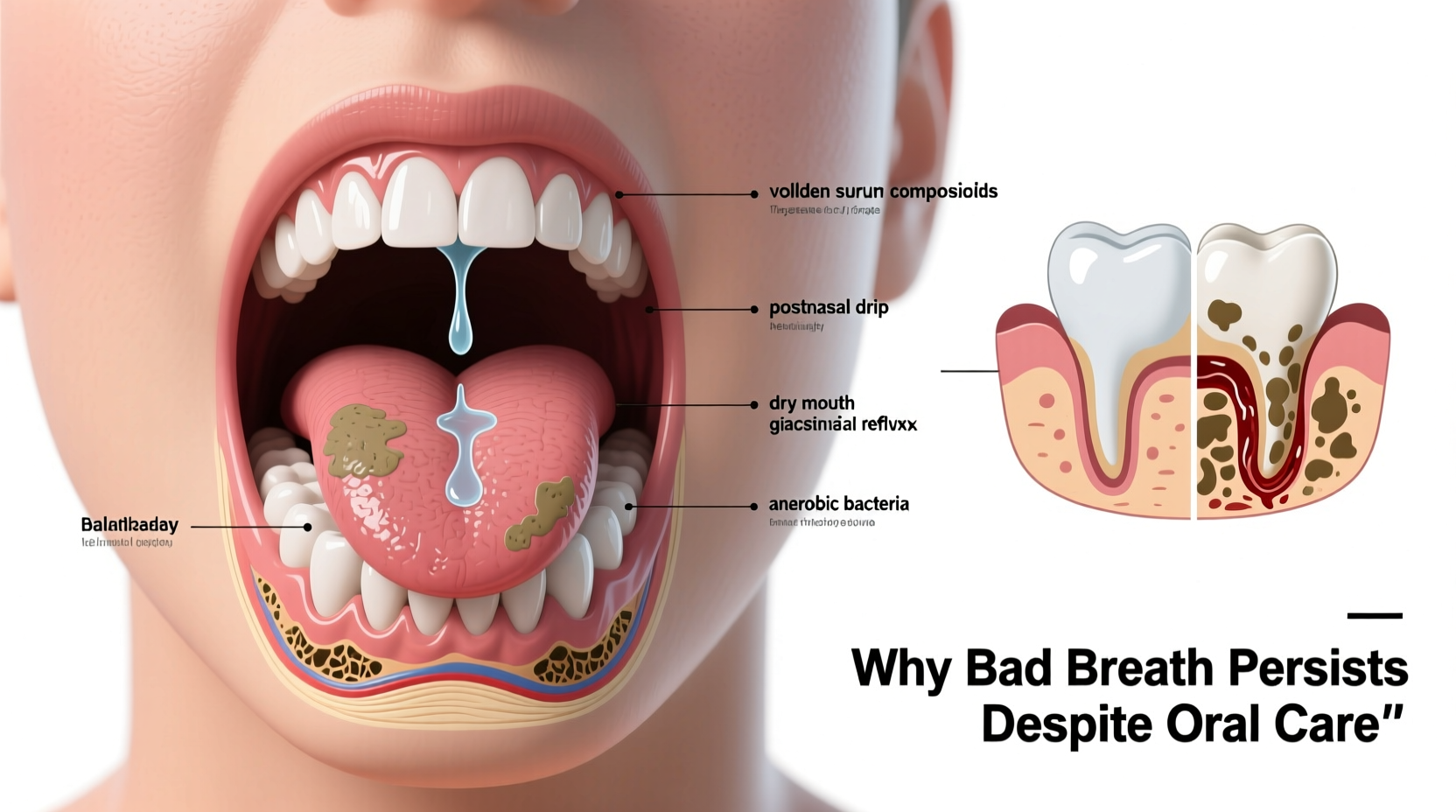
Even with excellent dental care, bad breath can persist due to factors that aren't always visible in the mirror. One of the most overlooked sources is the back of the tongue. While brushing teeth removes plaque and food debris from the front surfaces, many people neglect the tongue—especially its posterior third, where anaerobic bacteria thrive in the deep crevices of the papillae. These bacteria break down proteins in dead cells and mucus, releasing volatile sulfur compounds (VSCs) like hydrogen sulfide and methyl mercaptan—the primary culprits behind foul odors.
Dry mouth, medically known as xerostomia, is another major contributor. Saliva acts as a natural cleanser, neutralizing acids and washing away food particles and bacteria. When saliva production drops—due to medications, dehydration, sleep, or medical conditions—bacteria multiply rapidly, leading to odor buildup. Over 400 medications, including antihistamines, antidepressants, and blood pressure drugs, list dry mouth as a side effect.
Sinus and Respiratory Conditions That Trigger Bad Breath
Nasal and sinus issues are often silent contributors to persistent bad breath. Postnasal drip, for example, occurs when excess mucus drips down the back of the throat. This mucus provides a rich protein source for bacteria, which then produce foul-smelling byproducts. Chronic sinus infections, allergies, and even non-allergic rhinitis can increase mucus production and create an ideal environment for odor development.
Similarly, respiratory tract infections such as bronchitis, pneumonia, or tonsillitis may lead to bad breath. Infections in the tonsils can form tonsil stones—small, calcified masses trapped in the tonsillar crypts. These stones emit a rotten egg smell due to bacterial decomposition and are often undetected unless dislodged or seen during a medical exam.
“Many patients come in convinced their brushing isn’t good enough, but the real issue lies in postnasal drip or tonsil involvement. It’s not about effort—it’s about targeting the right source.” — Dr. Alan Foster, Otolaryngologist
Gastrointestinal and Systemic Health Connections
The digestive system can also play a role in breath odor. Gastroesophageal reflux disease (GERD), for instance, causes stomach acid and partially digested food to rise into the esophagus and mouth. This regurgitation introduces acidic, foul-smelling vapors that brushing alone cannot eliminate. People with GERD often report a sour or bitter taste along with persistent bad breath, especially in the morning.
Other systemic conditions linked to halitosis include diabetes (which may produce a fruity or acetone-like odor due to ketoacidosis), liver failure (musty or \"fishy\" breath), and kidney disease (ammonia-like odor). While these are less common, they underscore the importance of viewing bad breath as a potential symptom rather than just a cosmetic issue.
| Condition | Associated Breath Odor | Notes |
|---|---|---|
| GERD / Acid Reflux | Sour, acidic | Worse after meals or lying down |
| Diabetes (Ketoacidosis) | Fruity, nail polish remover | Requires urgent medical attention |
| Liver Dysfunction | Musty, sweet, or fishy | Known as \"fetor hepaticus\" |
| Chronic Kidney Disease | Ammonia-like, urine-like | Due to urea breakdown in saliva |
Hidden Dental Issues Behind Persistent Odor
Even diligent brushing and flossing can miss underlying dental problems. Gum disease (periodontitis) is one of the most common yet underdiagnosed causes of chronic bad breath. It begins with plaque buildup below the gumline, leading to inflammation, pocket formation, and bacterial colonies that release VSCs. Unlike surface plaque, these pockets are inaccessible to regular brushing and require professional cleaning.
Tooth decay, cracked fillings, abscesses, and poorly fitting dental appliances can also trap food and bacteria, creating localized odor sources. Some people develop “dry socket” after extractions, or retain food in orthodontic brackets or dentures, both of which contribute to persistent halitosis despite apparent hygiene.
A Real-Life Example: Sarah’s Story
Sarah, a 34-year-old teacher, brushed and flossed religiously and used alcohol-free mouthwash twice daily. Still, she noticed coworkers subtly stepping back during conversations. Embarrassed, she visited her dentist, who found moderate periodontitis and deep gum pockets harboring bacteria. After scaling and root planing (deep cleaning), along with a prescription antimicrobial rinse, her breath improved dramatically within two weeks. Sarah hadn’t realized that her bleeding gums were a sign of infection contributing to odor—proof that even meticulous routines can miss clinical issues.
Step-by-Step Guide to Diagnose and Treat Hidden Causes
If your breath remains offensive despite good hygiene, follow this systematic approach to identify and resolve the root cause:
- Evaluate your tongue and saliva levels: Check for a white or yellow coating on the tongue and symptoms of dry mouth (sticky feeling, frequent thirst).
- Review medications: Look up any prescriptions or over-the-counter drugs you take to see if dry mouth is a listed side effect.
- Assess nasal and sinus health: Note if you have frequent congestion, postnasal drip, or sinus infections.
- Monitor digestive symptoms: Track heartburn, regurgitation, bloating, or changes in appetite that might suggest GERD or other GI issues.
- Schedule a dental exam: Request a periodontal evaluation, including probing depths and X-rays to check for hidden decay or bone loss.
- Consult a physician if needed: If oral and ENT causes are ruled out, consider blood work to check for diabetes, liver, or kidney function.
Do’s and Don’ts for Long-Term Breath Management
| Do’s | Don’ts |
|---|---|
| Use a tongue scraper daily | Ignore bleeding gums |
| Stay hydrated throughout the day | Smoke or use tobacco products |
| Chew sugar-free gum to stimulate saliva | Overuse alcohol-based mouthwashes |
| Eat crunchy fruits and vegetables to naturally clean teeth | Self-diagnose serious systemic causes |
| Replace your toothbrush every 3 months | Skip regular dental cleanings |
Checklist: Is Your Routine Missing a Key Element?
- ✅ Brush teeth and gums for two minutes, twice daily
- ✅ Floss between all teeth daily
- ✅ Clean your tongue with a scraper, not just a brush
- ✅ Use a non-alcoholic, antibacterial mouthwash
- ✅ Drink water regularly, especially after meals
- ✅ Visit your dentist every 6 months for a cleaning and checkup
- ✅ Evaluate medications for dry mouth side effects
- ✅ Address persistent nasal congestion or acid reflux
FAQ: Common Questions About Persistent Bad Breath
Can probiotics help with bad breath?
Yes, emerging research suggests that certain oral probiotics, such as Streptococcus salivarius K12, can help crowd out odor-causing bacteria in the mouth and throat. These supplements are available as lozenges and may support microbial balance, especially after antibiotic use or in cases of recurrent tonsil stones.
Is morning breath normal?
Morning breath is common due to reduced saliva flow during sleep, allowing bacteria to proliferate. However, if the odor is extremely strong or lingers long after waking, it may indicate an underlying issue like sleep apnea, chronic dry mouth, or untreated gum disease.
Why does my breath smell bad even after using mouthwash?
Mouthwash can mask odor temporarily but doesn’t eliminate the source if it’s coming from deep gum pockets, the back of the tongue, sinuses, or internal health issues. Alcohol-based rinses may even worsen dry mouth, increasing bacterial growth over time. Opt for therapeutic rinses with cetylpyridinium chloride, chlorhexidine, or zinc ions for longer-lasting results.
Conclusion: Take Control of Your Breath Confidence
Persistent bad breath despite brushing, flossing, and using mouthwash is more common than you think—and rarely a reflection of poor effort. The causes are often hidden: from tongue biofilm and dry mouth to sinus drainage, gastrointestinal reflux, or undiagnosed dental disease. By broadening your understanding beyond surface hygiene, you can target the real source of the problem. Start with a comprehensive dental checkup, evaluate your overall health, and refine your daily routine with targeted strategies like tongue scraping and hydration. Fresh breath isn’t just about minty freshness—it’s a sign of holistic oral and systemic wellness.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?