The whites of your eyes—also known as the sclera—can turn red due to a variety of reasons, ranging from minor irritations to serious eye conditions. While occasional redness may not be alarming, persistent or painful redness can signal an underlying issue that requires prompt attention. Understanding what causes redness in the eye’s white area and recognizing when it's time to consult a healthcare provider can prevent complications and preserve vision.
Common Causes of Red Eyes
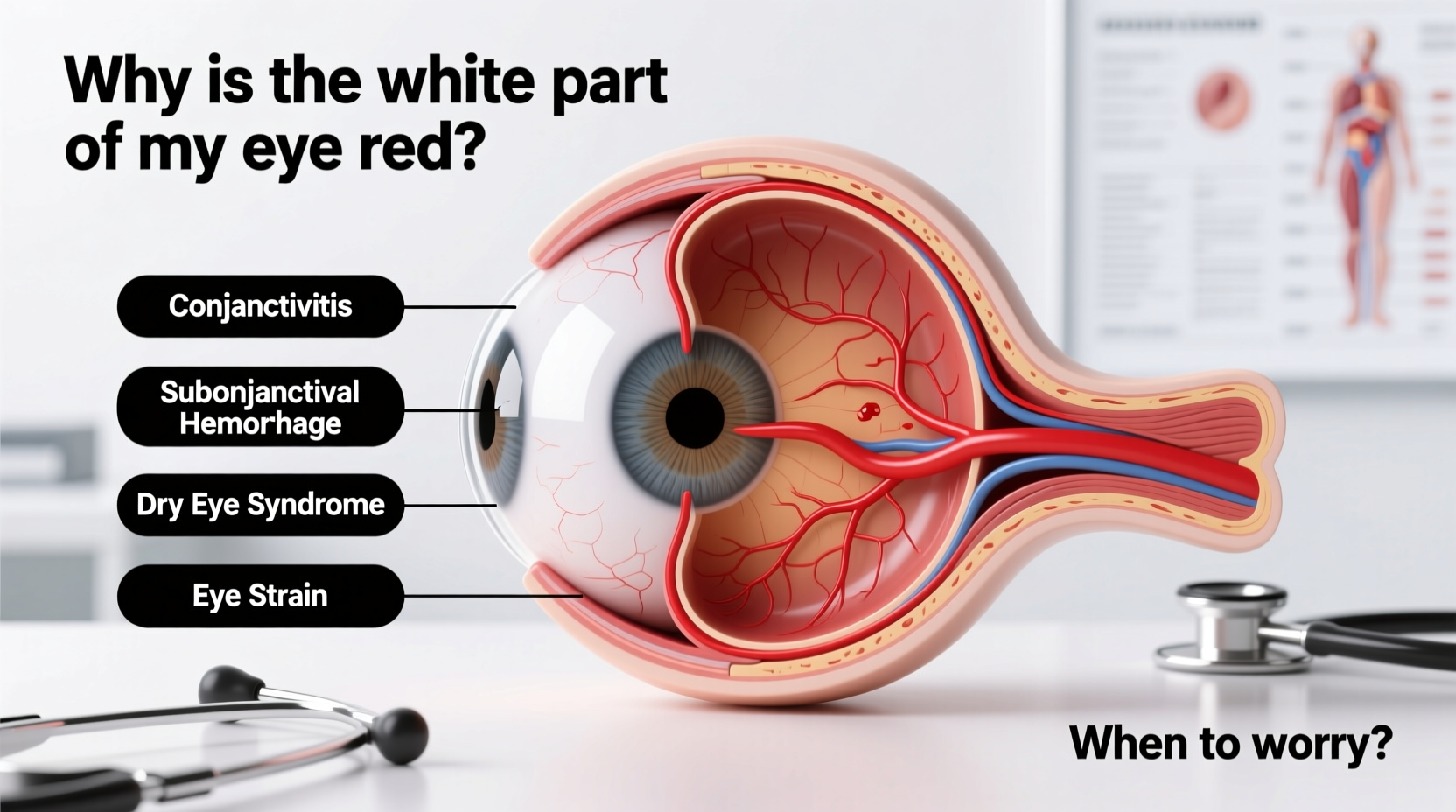
Redness in the sclera typically results from dilated or swollen blood vessels on the surface of the eye. These vessels are located in the conjunctiva, the thin, transparent layer covering the sclera. When irritated or inflamed, they become more visible, giving the eye a reddened appearance.
- Dry Eye Syndrome: Insufficient tear production or poor tear quality leads to dryness, irritation, and redness. This is especially common in people who spend long hours in front of screens or in air-conditioned environments.
- Allergies: Seasonal allergens like pollen, dust, or pet dander trigger histamine release, causing itching, swelling, and redness. Allergic conjunctivitis often affects both eyes.
- Eye Strain: Prolonged reading, driving, or digital screen use can fatigue the eyes, leading to temporary redness and discomfort.
- Foreign Body or Irritation: A speck of dust, eyelash, or contact lens debris can cause localized redness and tearing until flushed out.
- Subconjunctival Hemorrhage: A bright red patch appears when a small blood vessel breaks under the conjunctiva. Though it looks alarming, it’s usually painless and resolves on its own within one to two weeks.
- Smoke or Environmental Irritants: Exposure to smoke, chlorine in pools, strong perfumes, or chemical fumes can cause transient redness.
When Redness Signals a Serious Condition
Not all red eyes are harmless. Some conditions involve deeper inflammation or infection and require immediate evaluation by an eye care professional. These include:
- Bacterial or Viral Conjunctivitis (Pink Eye): Highly contagious, this condition causes redness, discharge (yellow/green for bacterial, watery for viral), and crusting of eyelids. It spreads easily through touch or shared items.
- Uveitis: Inflammation of the uvea (middle layer of the eye) causes deep redness around the iris, light sensitivity, blurred vision, and pain. It can be associated with autoimmune disorders or infections.
- Acute Glaucoma (Angle-Closure Glaucoma): A medical emergency where intraocular pressure spikes rapidly. Symptoms include severe eye pain, redness, nausea, halos around lights, and sudden vision loss.
- Keratitis: Corneal inflammation, often due to infection (especially in contact lens wearers), trauma, or dryness. Presents with pain, redness, tearing, and decreased vision.
- Scleritis: Severe inflammation of the sclera itself. Often linked to autoimmune diseases like rheumatoid arthritis. Characterized by intense, boring pain that may worsen at night.
“Any red eye accompanied by pain, vision changes, or photophobia should be evaluated immediately. Delaying care can lead to permanent vision damage.” — Dr. Alan Reyes, Ophthalmologist
Do’s and Don’ts: Managing Red Eye at Home
| Do’s | Don’ts |
|---|---|
| Use artificial tears for dryness or irritation | Do not rub your eyes aggressively |
| Apply a cold compress to reduce swelling | Avoid wearing contact lenses until symptoms resolve |
| Wash hands frequently if you have pink eye | Never share towels, eye drops, or makeup |
| Take screen breaks every 20 minutes (20-20-20 rule) | Do not use over-the-counter redness-relief drops daily |
| Keep the environment humidified during dry seasons | Avoid swimming in chlorinated pools with red eyes |
Real-Life Example: Recognizing a Medical Emergency
Sarah, a 45-year-old teacher, noticed her right eye becoming increasingly red and painful one evening. She initially assumed it was due to fatigue from grading papers. By morning, she experienced blurred vision, saw rainbow-colored halos around lights, and felt nauseous. Her husband urged her to visit an urgent eye clinic. The ophthalmologist diagnosed acute angle-closure glaucoma and immediately administered medication to lower her eye pressure. Thanks to timely intervention, Sarah avoided permanent optic nerve damage. This case underscores how quickly a red eye can escalate into a sight-threatening condition.
Step-by-Step Guide: What to Do If Your Eye Is Red
- Assess Symptoms: Note whether the redness is isolated or widespread, if there’s pain, discharge, vision changes, or light sensitivity.
- Check for Triggers: Consider recent exposure to allergens, prolonged screen time, contact lens use, or potential injury.
- Practice Gentle Care: Rinse eyes with clean water or saline solution. Use lubricating drops if dryness is suspected.
- Monitor Progress: Reassess after 24 hours. If redness persists or worsens, discontinue self-treatment.
- Seek Professional Help: Contact an optometrist or ophthalmologist if you experience pain, vision issues, or signs of infection.
FAQ: Frequently Asked Questions About Red Eyes
Can high blood pressure cause red eyes?
High blood pressure alone rarely causes noticeable eye redness. However, extremely elevated pressure may contribute to subconjunctival hemorrhage. More commonly, hypertension affects the retina over time, which requires specialized examination.
Is it safe to use redness-relief eye drops regularly?
No. Drops containing vasoconstrictors like tetrahydrozoline reduce redness temporarily but can cause rebound hyperemia—worsening redness upon discontinuation—with frequent use. Limit their use to short-term relief and consult a doctor for chronic redness.
How long does a subconjunctival hemorrhage last?
Most cases resolve within 10 to 14 days without treatment. The blood gradually clears, similar to a bruise. No specific therapy is needed unless recurrent episodes occur, which may warrant further investigation.
Conclusion: Prioritize Eye Health Before It’s Too Late
Redness in the white part of the eye is common, but it should never be ignored when accompanied by pain, vision changes, or systemic symptoms. While many causes are benign and self-limiting, others demand urgent medical attention to prevent irreversible damage. Being proactive—knowing the warning signs, avoiding harmful habits, and seeking timely care—can protect your vision for years to come.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?