Polycystic Ovary Syndrome (PCOS) affects approximately 1 in 10 women of reproductive age, yet up to 70% remain undiagnosed. This hormonal disorder is not only a leading cause of infertility but also increases the risk of type 2 diabetes, cardiovascular disease, and mental health challenges. Early recognition and proper diagnosis are critical. Unfortunately, symptoms vary widely, and many are mistaken for unrelated issues. This guide breaks down what PCOS really looks like, how to track your signs effectively, and the steps to secure a reliable diagnosis from healthcare professionals.
Understanding PCOS: More Than Just Cysts
The term “polycystic ovaries” can be misleading. While some women with PCOS have multiple small follicles on their ovaries visible via ultrasound, others do not. The core issue lies in hormonal imbalance—specifically elevated levels of androgens (male hormones), irregular ovulation, and insulin resistance. According to the Rotterdam Criteria, used globally for diagnosis, at least two of the following three must be present:
- Irregular or absent menstrual cycles
- Signs of high androgen levels (clinical or blood test)
- Polycystic ovaries on ultrasound
It’s important to note that having ovarian cysts does not automatically mean you have PCOS, and conversely, you can have PCOS without visible cysts.
“PCOS is a syndrome, not a single disease. Its presentation varies so much that we often see delays in diagnosis simply because providers expect a textbook case.” — Dr. Lena Patel, Endocrinologist and Women’s Health Specialist
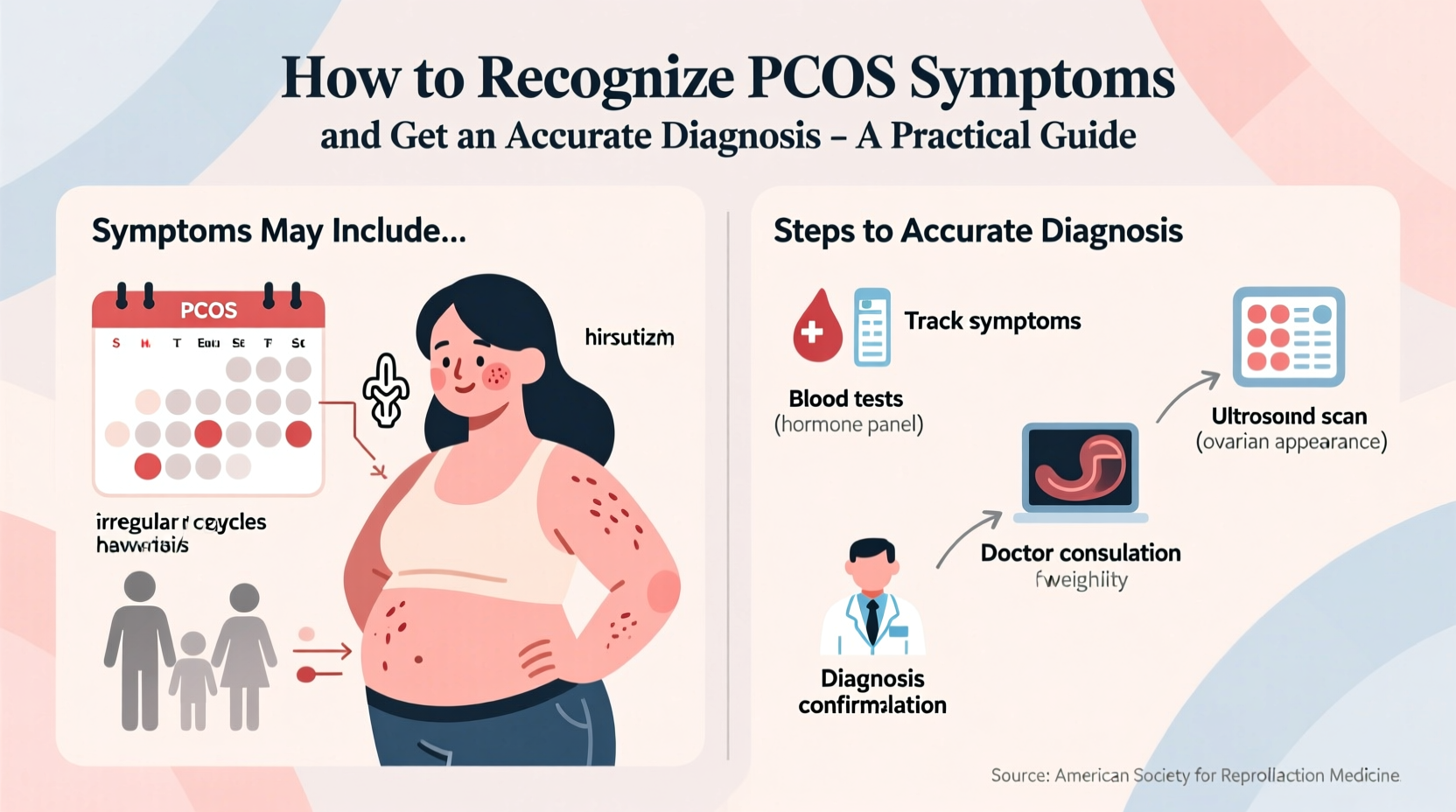
Common Symptoms and How to Track Them
Symptoms often begin shortly after puberty but may emerge in late teens or early adulthood. Because they develop gradually, many women dismiss them as normal variations of health. Recognizing patterns over time is key.
Physical and Hormonal Signs
- Irregular periods: Cycles longer than 35 days, fewer than eight periods per year, or complete absence (amenorrhea).
- Hirsutism: Excess hair growth on the face, chest, back, or abdomen due to high androgens.
- Acne: Persistent breakouts on the lower face, jawline, or neck, often resistant to topical treatments.
- Weight gain or difficulty losing weight: Especially around the abdomen, linked to insulin resistance.
- Thinning hair or hair loss: Male-pattern baldness or noticeable shedding at the crown.
- Acanthosis nigricans: Darkened skin patches on the neck, groin, or underarms—often a sign of insulin issues.
Metabolic and Emotional Indicators
PCOS doesn’t just affect reproduction. Many women experience fatigue, sugar cravings, and mood fluctuations. Anxiety and depression are more common in those with PCOS, partly due to hormonal shifts and partly due to the emotional toll of chronic symptoms.
Step-by-Step: How to Pursue a Diagnosis
Getting diagnosed with PCOS requires more than a single blood test or scan. It involves a combination of clinical evaluation, lab work, and imaging. Follow these steps to ensure a thorough assessment.
- Document your medical history: Note when your periods started, cycle regularity, weight changes, acne, and family history of PCOS, diabetes, or infertility.
- Schedule a visit with a gynecologist or endocrinologist: Choose a provider familiar with hormonal disorders. Primary care doctors may miss subtle signs.
- Request specific blood tests: These should include:
- Fasting glucose and insulin levels
- HbA1c (for long-term blood sugar control)
- Testosterone and DHEA-S (androgen markers)
- LH and FSH ratio (often elevated LH in PCOS)
- Thyroid panel (to rule out similar symptoms)
- Prolactin (elevated levels mimic PCOS)
- Undergo a pelvic ultrasound: A transvaginal scan evaluates ovarian morphology. However, this isn't always necessary if other criteria are met, especially in adolescents.
- Rule out other conditions: Your doctor should exclude thyroid dysfunction, hyperprolactinemia, and non-classical congenital adrenal hyperplasia.
Do’s and Don’ts When Seeking a Diagnosis
| Do’s | Don’ts |
|---|---|
| Track your menstrual cycle for at least 3 months before your appointment | Assume irregular periods are normal just because you’re young |
| Bring a list of all symptoms—even seemingly minor ones | Downplay concerns like excess hair or acne; they matter clinically |
| Ask for copies of your lab results and ultrasound report | Rely solely on online symptom checkers for diagnosis |
| Seek a second opinion if dismissed without testing | Accept birth control as the only solution without further investigation |
Real-Life Example: Delayed Diagnosis Despite Clear Symptoms
Sophia, a 24-year-old graphic designer, had struggled with acne since high school and began missing periods by age 19. Her GP prescribed birth control pills for \"cycle regulation\" but never investigated further. Over the next five years, she gained 30 pounds despite dieting and exercise, developed facial hair, and felt constantly fatigued. It wasn’t until she sought help for infertility that an endocrinologist ordered a full hormone panel and ultrasound. She was finally diagnosed with PCOS and insulin resistance. With medication and lifestyle changes, her cycles normalized within six months.
Sophia’s story reflects a common pattern: symptom normalization by both patients and providers. Had she been screened earlier, she might have avoided years of metabolic strain and emotional distress.
Essential Checklist Before Your Doctor’s Visit
Prepare thoroughly to make the most of your consultation. Use this checklist to gather essential information:
- 📅 Menstrual calendar (dates of last 6–12 periods)
- 📝 Symptom log (acne, hair growth, mood, sleep, weight trends)
- 📋 Family history (diabetes, PCOS, infertility)
- 💉 List of medications and supplements
- ❓ Questions for your doctor (e.g., “Could my acne be hormonal?” or “Should I be tested for insulin resistance?”)
- 📊 Request copies of all test results for your records
Frequently Asked Questions
Can you have PCOS without weight gain?
Yes. While about 80% of women with PCOS are overweight or obese, 20% are lean. Lean PCOS may present with milder symptoms, making diagnosis harder. Irregular periods and elevated androgens are still key indicators.
Is PCOS curable?
There is no cure, but it is highly manageable. Lifestyle changes—especially balanced nutrition, regular movement, and stress reduction—can significantly reduce symptoms. Medications like metformin or oral contraceptives help regulate cycles and hormones.
Does PCOS go away after menopause?
Hormonal imbalances persist, though menstrual symptoms resolve. Risks for diabetes and heart disease remain elevated, so ongoing monitoring is important even post-menopause.
Conclusion: Take Charge of Your Health
Recognizing PCOS starts with trusting your body and questioning persistent abnormalities. Too many women suffer in silence, told their symptoms are “just part of being a woman.” But irregular periods, stubborn acne, and unexplained weight gain are not normal—they are signals. By tracking your symptoms, advocating for comprehensive testing, and seeking informed care, you can obtain an accurate diagnosis and take meaningful steps toward better health. Whether you're trying to conceive, manage weight, or simply feel like yourself again, clarity begins with action.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?