The color of your stool may seem like a trivial detail, but it’s actually one of the most telling indicators of your digestive health. Most people expect their bowel movements to be brown—and for good reason. That familiar hue isn’t random; it’s the result of complex biological processes involving bile, bilirubin, and gut bacteria. However, stool color can vary significantly due to diet, medications, or underlying health conditions. Understanding what different colors mean empowers you to recognize normal fluctuations from potential red flags.
The Science Behind Brown Stool
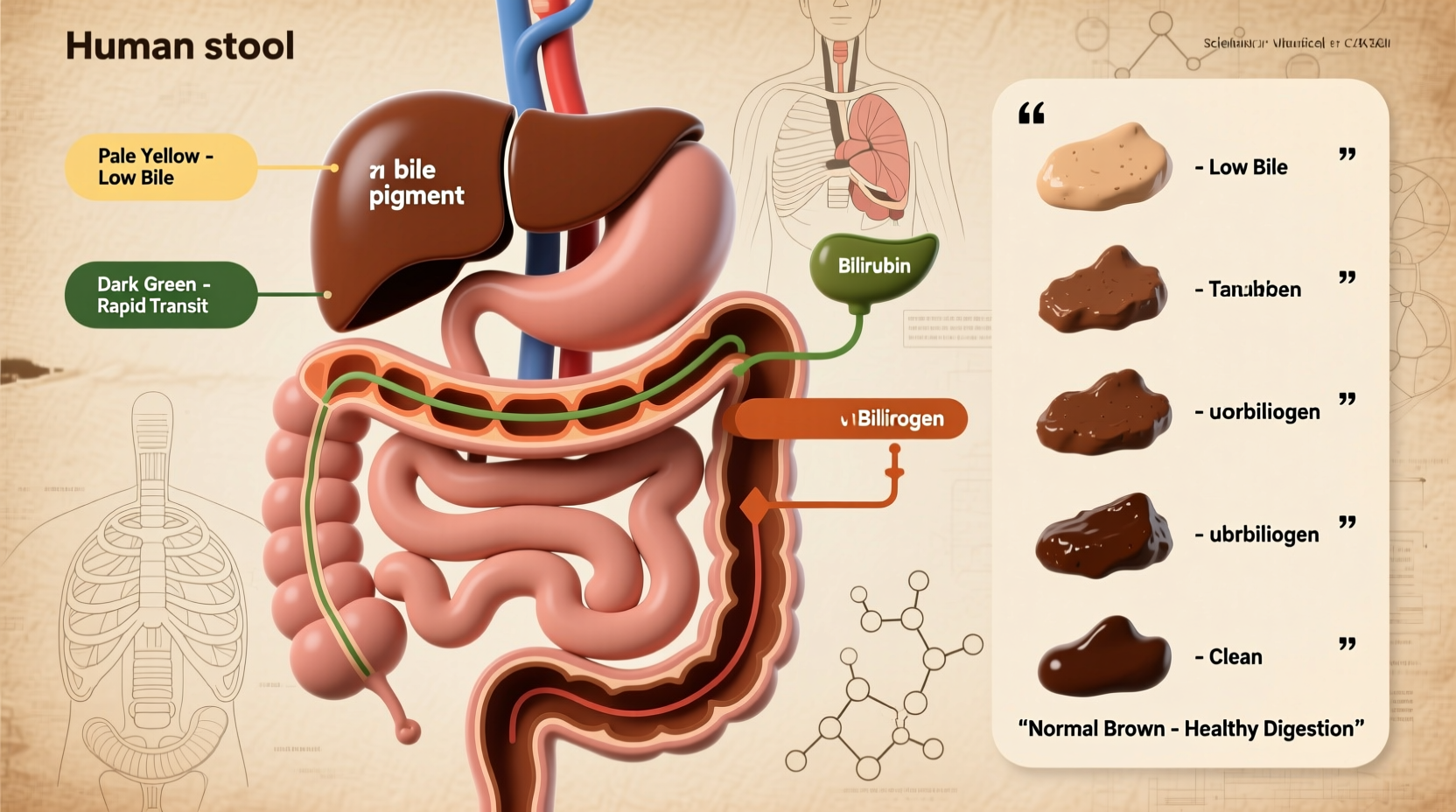
Brown stool is the norm because of how your body processes red blood cells. When old red blood cells are broken down in the spleen, they release hemoglobin. The liver converts hemoglobin into a substance called bilirubin, which is then stored in the gallbladder as part of bile. Bile is released into the small intestine during digestion to help break down fats.
As bile travels through the intestines, gut bacteria metabolize bilirubin into urobilinogen. Some of this compound is reabsorbed and excreted in urine (giving it its yellow color), while the rest is further oxidized into stercobilin—the pigment responsible for the brown color of stool. This entire process is a finely tuned system, and any disruption can alter stool color.
Common Stool Colors and What They Mean
While brown is standard, other colors aren’t always cause for alarm. Here’s a breakdown of common stool colors and their possible causes:
| Color | Possible Causes | When to Be Concerned |
|---|---|---|
| Green | Leafy greens, food coloring, rapid transit through intestines (diarrhea), iron supplements | If persistent without dietary explanation or accompanied by discomfort |
| Yellow | High-fat diet, giardia infection, celiac disease, pancreatic issues | If greasy, foul-smelling, and recurrent—could indicate malabsorption |
| Black (tarry) | Iron supplements, bismuth (Pepto-Bismol), upper gastrointestinal bleeding | If not explained by medication and stool is sticky or foul-smelling—seek immediate care |
| Red | Beets, tomatoes, red food dye, hemorrhoids, lower GI bleeding | If bright red blood appears regularly or is unexplained—get evaluated |
| Clay/White/Pale | Lack of bile due to liver disease, gallstones, or bile duct obstruction | If persistent—requires prompt medical investigation |
| Blue | Rare; usually from artificial dyes in foods or drinks | Not medically significant unless recurring without dietary cause |
When Color Changes Are Normal
Short-term changes in stool color often reflect what you’ve eaten. For example, eating large amounts of spinach or kale can turn stool green, while blueberries might tint it dark purple. These shifts are harmless if they resolve within a day or two. Similarly, certain medications like antacids containing aluminum hydroxide may lighten stool, while antibiotics can temporarily alter gut flora and affect color.
Medical Conditions Linked to Abnormal Stool Color
Persistent deviations from brown stool may signal underlying conditions. Here are key associations:
- Clay-colored stools suggest a blockage in the bile ducts or impaired liver function. Conditions such as hepatitis, cirrhosis, or gallstones can reduce bile delivery to the intestines.
- Black, tarry stools (melena) often point to bleeding in the upper gastrointestinal tract—such as stomach ulcers or esophageal varices. The black color results from digested blood interacting with intestinal enzymes.
- Bright red blood mixed with or coating stool usually originates from the lower colon or rectum. Common causes include hemorrhoids, anal fissures, diverticulosis, or inflammatory bowel disease (IBD).
- Yellow, greasy stools that float and are difficult to flush may indicate fat malabsorption, seen in chronic pancreatitis, cystic fibrosis, or celiac disease.
“Stool color is a window into the digestive system. While occasional variation is normal, persistent changes—especially pale or black stools—should never be ignored.” — Dr. Lena Torres, Gastroenterologist, Mayo Clinic
Mini Case Study: Recognizing a Hidden Health Issue
Mark, a 48-year-old office worker, noticed his stool had turned pale gray over three weeks. He initially dismissed it, assuming it was due to a new multivitamin. However, he began experiencing mild fatigue and occasional itching. His primary care physician ordered liver function tests and an abdominal ultrasound, which revealed a partially obstructed bile duct caused by a small gallstone. After a minimally invasive procedure to remove the stone, Mark’s stool returned to normal within days. This case highlights how a seemingly minor change in stool color led to the early detection of a potentially serious condition.
Step-by-Step Guide: Evaluating Your Stool Color
If you notice an unusual stool color, follow this logical sequence to determine whether action is needed:
- Assess recent diet and medications. Did you consume beets, iron supplements, or brightly colored foods? Review any new prescriptions or over-the-counter drugs.
- Monitor frequency and consistency. Is the color isolated or ongoing? Use the Bristol Stool Scale as a reference for texture and form.
- Check for accompanying symptoms. Look for abdominal pain, bloating, weight loss, nausea, jaundice, or blood in stool.
- Wait 24–48 hours. If the color returns to normal and no symptoms persist, it was likely dietary.
- Consult a healthcare provider. If abnormal color continues beyond two days without explanation—or if you have concerning symptoms—schedule an appointment.
Checklist: When to Seek Medical Attention
Use this checklist to determine if a stool color change warrants professional evaluation:
- ☑ Persistent pale, white, or clay-colored stools (more than 1–2 bowel movements)
- ☑ Black, tarry stools not explained by medication or supplements
- ☑ Bright red blood in or on stool lasting more than a day
- ☑ Yellow, greasy, floating stools with foul odor occurring regularly
- ☑ Jaundice (yellowing of skin or eyes) alongside color changes
- ☑ Unexplained weight loss, abdominal pain, or fatigue with stool changes
FAQ
Can dehydration change stool color?
Dehydration primarily affects stool consistency, making it harder and darker brown due to increased concentration. It doesn’t typically cause dramatic color shifts like red, black, or white. However, severely dehydrated individuals may notice very dark stools, which should improve with fluid intake.
Is green poop dangerous?
Green stool is rarely dangerous. It often results from chlorophyll in leafy greens or food dyes. Rapid intestinal transit—common during diarrhea—can also prevent full bile breakdown, leaving stool green. Unless it persists or is accompanied by cramping, fever, or blood, green stool is usually benign.
Why do babies have different colored poop?
Infant stool varies widely. Newborns pass meconium (black, tarry stool) in the first few days. Breastfed babies often have yellow, seedy stools, while formula-fed infants may have tan or brown ones. Occasional green is normal. Parents should consult a pediatrician if there’s red streaks (possible allergy or fissure), white stools (liver issue), or signs of distress.
Conclusion
Stool color is far more than a bathroom curiosity—it’s a direct reflection of your internal health. The typical brown hue comes from bilirubin transformation via bile and gut bacteria, but deviations can reveal dietary habits, medication effects, or hidden medical issues. By paying attention to color, consistency, and associated symptoms, you gain valuable insight into your digestive system. Don’t ignore persistent changes, especially those involving black, white, or bloody stools. Early awareness leads to timely intervention, potentially preventing complications. Stay informed, stay observant, and prioritize open conversations with your healthcare provider about even the most uncomfortable topics.









 浙公网安备
33010002000092号
浙公网安备
33010002000092号 浙B2-20120091-4
浙B2-20120091-4
Comments
No comments yet. Why don't you start the discussion?